A ‘smart’ patch that automatically delivers insulin when needed
January 20, 2017
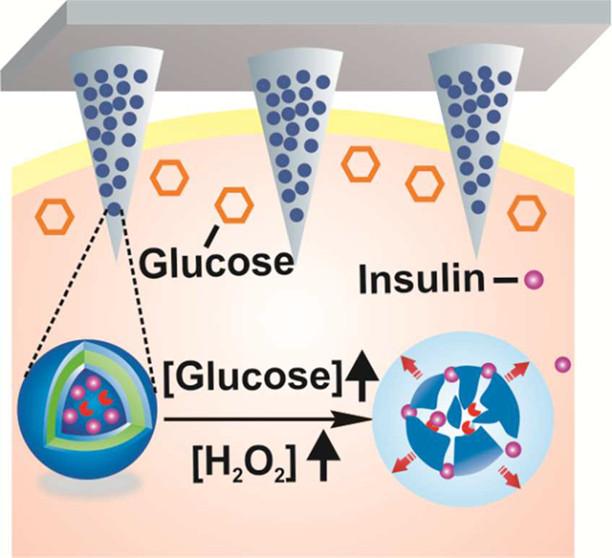
Tiny, painless microneedles on a patch can deliver insulin in response to rising glucose levels (credit: American Chemical Society)
A team of scientists has invented a replacement for daily glucose-level finger-pricking and insulin shots: a painless “smart” patch that monitors blood glucose and releases insulin when levels climb too high.
The report on the device, which has only been tested on mice so far, appears in the journal ACS Nano.
People with Type 1 diabetes don’t make insulin — a hormone that regulates blood glucose (sugar). Those with Type 2 diabetes can’t use insulin effectively. Either way, glucose builds up in the blood, which can lead to a host of health problems, including heart disease, stroke, blindness and amputation of toes, feet or legs.
To avoid these outcomes, people with Type 1 or advanced Type 2 diabetes regularly prick their fingers to measure blood-sugar levels, and some patients must inject themselves with insulin when needed. But sometimes, despite a person’s vigilance, glucose levels can still get out of whack.
A skin patch with painless microneedles
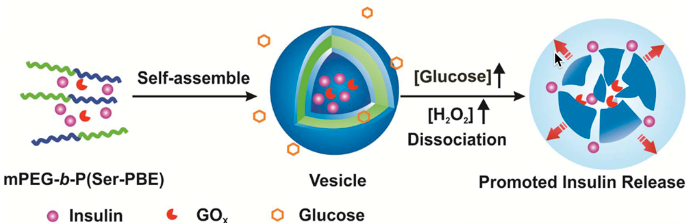
Self-assembly of block copolymer into vesicles loaded with insulin and glucose oxidase. The vesicles (engineered pouches) are dissociated to release insulin in the presence of a hyperglycemic state. (credit: American Chemical Society)
So Zhen Gu and colleagues* decided to invent a simpler, more effective, shot-free way to manage diabetes: a skin patch covered in painless microneedles that are loaded with tiny insulin-carrying pouches. The pouches (vesicles) are engineered to break apart rapidly and release the insulin in response to rising glucose levels.
Diabetic mice wearing the patch maintained consistent concentrations of insulin in their blood. When these mice received a shot of glucose, their blood sugar levels spiked initially, but then fell to normal levels within two hours.

Another automated approach: Insulin Pump Therapy system: 1. Insulin pump. 2: Flexible tubing delivers insulin from the pump reservoir to the infusion set. 3. A tiny tube called a cannula is inserted under your skin to deliver insulin. 4. Insulin in the blood (credit: Medtronics)
The authors acknowledge funding from the American Diabetes Association, National Institutes of Health, and the National Science Foundation.
* Affiliated with the University of North Carolina at Chapel Hill, North Carolina State University, and State Key Laboratory of Polymer Chemistry and Physics, Changchun Institute of Applied Chemistry, Chinese Academy of Sciences.
Abstract of H2O2-Responsive Vesicles Integrated with Transcutaneous Patches for Glucose-Mediated Insulin Delivery
A self-regulated “smart” insulin administration system would be highly desirable for diabetes management. Here, a glucose-responsive insulin delivery device, which integrates H2O2-responsive polymeric vesicles (PVs) with a transcutaneous microneedle-array patch was prepared to achieve a fast response, excellent biocompatibility, and painless administration. The PVs are self-assembled from block copolymer incorporated with polyethylene glycol (PEG) and phenylboronic ester (PBE)-conjugated polyserine (designated mPEG-b-P(Ser-PBE)) and loaded with glucose oxidase (GOx) and insulin. The polymeric vesicles function as both moieties of the glucose sensing element (GOx) and the insulin release actuator to provide basal insulin release as well as promote insulin release in response to hyperglycemic states. In the current study, insulin release responds quickly to elevated glucose and its kinetics can be modulated by adjusting the concentration of GOx loaded into the microneedles. In vivo testing indicates that a single patch can regulate glucose levels effectively with reduced risk of hypoglycemia.