Biocompatible interfaces replace silicon and metal in neural prosthetic devices
August 11, 2015
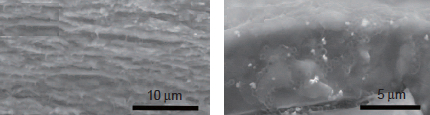
Left: collagen; right: matrigel (credit: Wen Shen et al./Microsystems & Nanoengineering)
Researchers at the University of Georgia’s Regenerative Bioscience Center have developed a biocompatible implantable neural prosthetic device to replace silicon and noble metal in neural prosthetic devices. The goal is to avoid immune-system rejection, failures due to tissue strain, neurodegeneration, and decreased fidelity of recorded neural signals.
Implantable neural prosthetic devices in the brain have been around for almost two decades, helping people living with limb loss and spinal cord injury become more independent, for example. They are also used for deep brain stimulation and brain-controlled prosthetic devices. However, existing neural prosthetic devices suffer from immune-system rejection, and most are believed to eventually fail because of a mismatch between the soft brain tissue and the rigid devices.
The researchers used a combination of a two materials as structural support for neural electrodes.
Collagen. Its higher mechanical strength can support initial insertion while softening after implantation. Collagen is an extracellular matrix environment (ECM) protein that is critical in the formation of connective structures in tendons, organs, and basement membranes in the body and features long fibrils and 3D structures with high tensile strengths. The ECM is a collection of molecules secreted by cells that provides structural and biochemical support to surrounding cells.
Matrigel, a gelatinous ECM protein mixture resembling the complex extracellular neuronal environment, used to provide a more neuronal-compatible substrate.
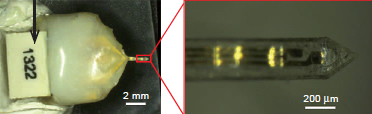
A representative extracellular matrix-based implantable neural electrode device and an enlarged view of the electrode tip (credit: Wen Shen et al./Microsystems & Nanoengineering)
“This is not by any means the device that you’re going to implant into a patient,” said Karumbaiah, an assistant professor of animal and dairy science in the UGA College of Agricultural and Environmental Sciences. “This is proof of concept that extracellular matrix can be used to ensheathe a functioning electrode without the use of any other foreign or synthetic materials.”
The collaboration, led by Wen Shen and Mark Allen of the University of Pennsylvania, found that the extracellular matrix derived electrodes adapted to the mechanical properties of brain tissue and were capable of acquiring neural recordings from the brain cortex.
Currently, one out of every 190 Americans is living with limb loss, according to the National Institutes of Health. There is a significant burden in cost of care and quality of life for people suffering from this disability.
The research is described in an open-access paper in the journal Microsystems & Nanoengineering.
Abstract of Extracellular matrix-based intracortical microelectrodes: Toward a microfabricated neural interface based on natural materials
Extracellular matrix (ECM)-based implantable neural electrodes (NEs) were achieved using a microfabrication strategy on natural-substrate-based organic materials. The ECM-based design minimized the introduction of non-natural products into the brain. Further, it rendered the implants sufficiently rigid for penetration into the target brain region and allowed them subsequently to soften to match the elastic modulus of brain tissue upon exposure to physiological conditions, thereby reducing inflammatory strain fields in the tissue. Preliminary studies suggested that ECM-NEs produce a reduced inflammatory response compared with inorganic rigid and flexible approaches. In vivo intracortical recordings from the rat motor cortex illustrate one mode of use for these ECM-NEs.