Controlling inflammation to reduce chronic disease risk
August 10, 2015
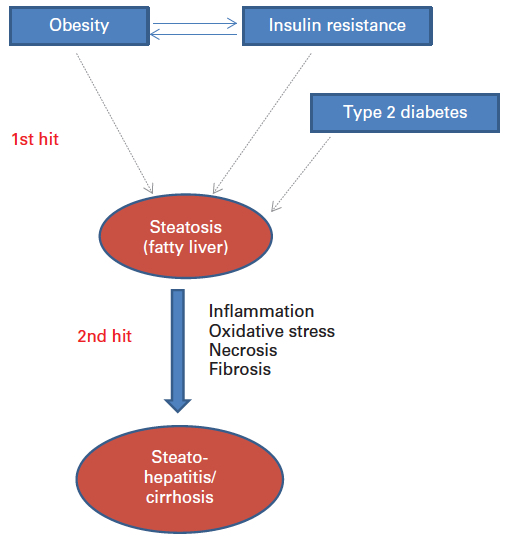
Two-hit model of non-alcoholic fatty liver disease (credit: ILSI Europe)
In an open-access paper in the British Journal of Nutrition, a coalition of 17 experts explain how elevated unresolved chronic inflammation is involved a range of chronic diseases, and how nutrition influences inflammatory processes and helps reduce chronic risk of diseases.
According to the authors, “the nutrition status of the individual with for example a deficiency or excess of certain micronutrients (e.g. folate, vitamin B12, vitamin B6, vitamin 1, vitamin E, zinc) may lead to an ineffective or excessive inflammatory response.
“Studies have showed that high consumption of fat and glucose may induce post-prandial inflammation (manifesting itself after the consumption of a meal), which may have consequences for the development of diabetes and cardiovascular diseases. The Western-style diet, rich in fat and simple sugars but often poor in specific micronutrients, is linked to the increased prevalence of diseases with strong immunogical and autoimmune components, including allergies, food allergies, atopic dermatitis and obesity.”
“Inflammation acts as both a friend and foe, being essential in metabolic regulation, with unresolved low-grade chronic inflammation being a pathological feature of a wide range of chronic conditions including the metabolic syndrome and cardiovascular diseases,” commented a co-author, Prof. Anne Marie Minihane, University of East Anglia (UK).
Abstract of Low-grade inflammation, diet composition and health: current research evidence and its translation
The importance of chronic low-grade inflammation in the pathology of numerous age-related chronic conditions is now clear. An unresolved inflammatory response is likely to be involved from the early stages of disease development. The present position paper is the most recent in a series produced by the International Life Sciences Institute’s European Branch (ILSI Europe). It is co-authored by the speakers from a 2013 workshop led by the Obesity and Diabetes Task Force entitled ‘Low-grade inflammation, a high-grade challenge: biomarkers and modulation by dietary strategies’. The latest research in the areas of acute and chronic inflammation and cardiometabolic, gut and cognitive health is presented along with the cellular and molecular mechanisms underlying inflammation–health/disease associations. The evidence relating diet composition and early-life nutrition to inflammatory status is reviewed. Human epidemiological and intervention data are thus far heavily reliant on the measurement of inflammatory markers in the circulation, and in particular cytokines in the fasting state, which are recognised as an insensitive and highly variable index of tissue inflammation. Potential novel kinetic and integrated approaches to capture inflammatory status in humans are discussed. Such approaches are likely to provide a more discriminating means of quantifying inflammation–health/disease associations, and the ability of diet to positively modulate inflammation and provide the much needed evidence to develop research portfolios that will inform new product development and associated health claims.