Drug-delivery nanoparticles mimic white blood cells to avoid immune rejection
February 4, 2013
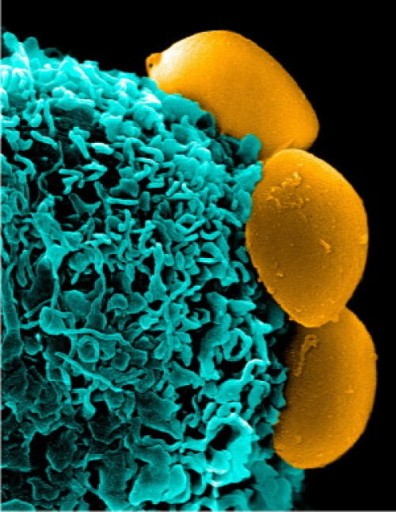
Camouflaged nanoparticles (yellow) cloaked in the membranes of white blood cells rest on the surface of an immune system cell (phagocyte, blue) without being recognized, ingested, and destroyed (credit: Methodist Hospital, Houston)
Scientists at The Methodist Hospital Research Institute have found a possible way to fool the immune system to prevent it from recognizing and destroying nanoparticles before they deliver their drug payloads.
“Our goal was to make a particle that is camouflaged within our bodies and escapes the surveillance of the immune system to reach its target undiscovered,” said Department of Medicine Co-Chair Ennio Tasciotti, Ph.D., the study’s principal investigator.
They accomplished that by using lipids and proteins present on the membrane of immune system leukocytes (white blood cells) to coat a nanoparticle to make the body’s immune system recognize these nanoparticles as its own.
(Nanoparticles can deliver different types of drugs to specific cell types, for example, chemotherapy to cancer cells. But the ability of the body’s defenses to destroy nanoparticles is a major barrier to the use of nanotechnology in medicine._
“Using the membranes of the white blood cells to coat a nanoparticle has never been done before,” Tasciotti said. “The leukolike vectors.(LLVs) are half man-made — the synthetic silicon core — and half made of man — the cell membrane.”
As the technology is further developed, a patient’s own white cells could be harvested and used to create personalized LLVs, Tasciotti said.
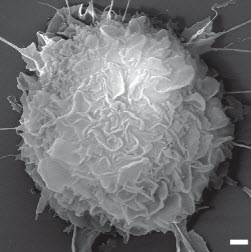
TEM image of a drug-containing nanoparticle covered with mimicked white blood cells (scale bar: 100 nm)
“LLVs are dotted with specific proteins that help the particles reach specific targets, such as inflamed or damaged tissues and cancer cells recruiting blood vessels,” Tasciotti said.
Once the nanoparticles reach their target tissue, the membrane lipids and proteins will break away in a controllable release, leaving the nanoparticles to degrade naturally after releasing their payload.
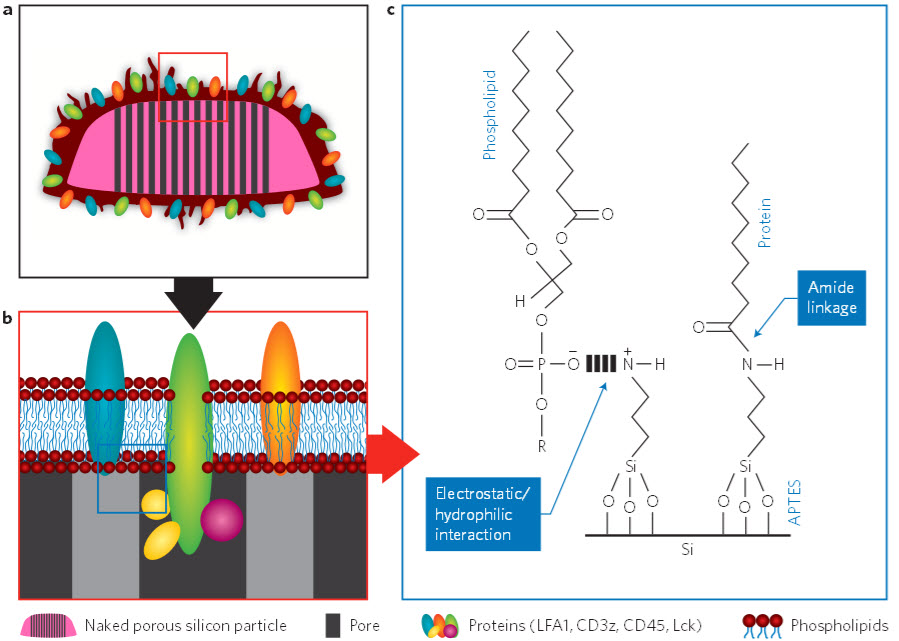
A cartoon of the leukocyte-like vector. (a) The leukocyte-like cell membranes fully cover the nanoporous
silicon platform (NPS) and seal off its pores. (b) Enlargement of the area outlined with the red box. (c) Schematic showing possible interactions between the APTES (a sort of binder) group on the NPS surface and a membrane phospholipid and protein. (Credit: Alessandro Parodi et al./Nature Nanotechnology)
Tasciotti is also the co-chair of the Department of Nanomedicine and is the director of the Surgical Advanced Technology Lab at The Methodist Hospital.
This work was funded by the U.S. Army’s Telemedicine & Advanced Technology Research Center, the U.S. Defense Advanced Research Projects Agency (DARPA), the National Institutes of Health, and the U.S. Department of Defense’s Breast Cancer Research Program.