Electrical signatures of consciousness in the dying brain
August 15, 2013

(Credit: iStockphoto)
A University of Michigan animal study shows that shortly after clinical death, in which the heart stops beating and blood stops flowing to the brain, rats display brain activity patterns characteristic of conscious perception.
The “near-death experience” (NDE) reported by cardiac arrest survivors worldwide may be grounded in science, according to research at the University of Michigan Health System.
“This study, performed in animals, is the first dealing with what happens to the neurophysiological state of the dying brain,” says lead study author Jimo Borjigin, Ph.D., associate professor of molecular and integrative physiology and associate professor of neurology at the University of Michigan Medical School.
“It will form the foundation for future human studies investigating mental experiences occurring in the dying brain, including seeing light during cardiac arrest,” she says.
Approximately 20 percent of cardiac arrest survivors report having had a near-death experience. These visions and perceptions have been called “realer than real,” according to previous research, but it has remained unclear whether the brain is capable of such activity after cardiac arrest.
Researchers have now analyzed the recordings of brain activity called electroencephalograms (EEGs) from nine anesthetized rats undergoing experimentally induced cardiac arrest.
Within the first 30 seconds after cardiac arrest, all of the rats displayed a widespread, transient surge of highly synchronized brain activity that had features associated with a highly aroused brain. They also displayed nearly identical patterns after undergoing asphyxiation.
“The prediction that we would find some signs of conscious activity in the brain during cardiac arrest was confirmed with the data,” says Borjigin, who conceived the idea for the project in 2007 with study co-author neurologist Michael M. Wang, M.D., Ph.D., associate professor of neurology and associate professor of molecular and integrative physiology at the U-M.
Higher levels of brain activity than in waking state
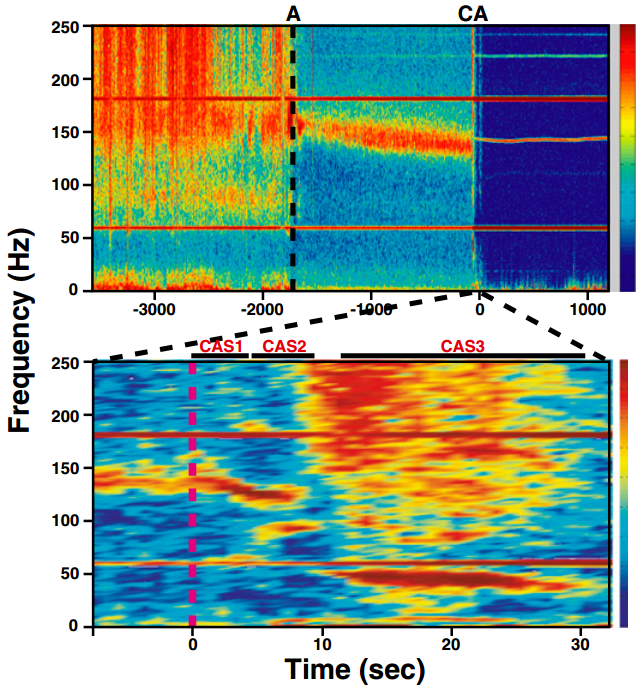
Mean gamma coherence values over six EEG channels during waking (30 min), anesthesia (30 min), and following cardiac arrest (20 min) are shown for one representative rat. A narrow window of sharply increased coherence occurs across all frequency bands and is clearly detectable immediately following cardiac arrest. An expanded analysis is shown in tje lower plot. Three distinct cardiac arrest states were detected: CAS1, CAS2, and CAS3, with blue indicating low levels of gamma coherence and red indicating high levels. (Credit: Jimo Borjigin et al./PNAS)
“But, we were surprised by the high levels of activity,” adds study senior author anesthesiologist George Mashour, M.D., Ph.D., assistant professor of anesthesiology and neurosurgery at the U-M. “
In fact, at near-death, many known electrical signatures of consciousness exceeded levels found in the waking state, suggesting that the brain is capable of well-organized electrical activity during the early stage of clinical death.
“We identified a transient surge of synchronous gamma oscillations that occurred within the first 30 seconds after cardiac arrest [that] preceded isoelectric [flatline] electroencephalogram.
Gamma oscillations are high-frequency brainwaves above 25 Hz. associated with waking consciousness, altered states of consciousness during meditation, and rapid eye movement (REM) sleep, the researchers explain.
“Gamma oscillations during cardiac arrest were global and highly coherent; moreover,
this frequency band exhibited a striking increase in anterior–posterior-directed connectivity … associated with conscious perception,” and “tight phase-coupling to both theta and alpha waves.
“Recent studies suggest that cross-frequency coupling between theta and gamma
rhythms may play a functional role in long-range neuronal communication, perception, and memory tasks.”
The brain is assumed to be inactive during cardiac arrest. However the neurophysiological state of the brain immediately following cardiac arrest had not been systemically investigated until now.
“This study tells us that reduction of oxygen or both oxygen and glucose during cardiac arrest can stimulate brain activity that is characteristic of conscious processing,” says Borjigin. “It also provides the first scientific framework for the near-death experiences reported by many cardiac arrest survivors.
“Internally generated visions and perceptions are also reported by ∼20% of cardiac arrest survivors during clinical death,” the researchers say in the PNAS paper.
Challenging ‘out-of-the-body’ consciousness
“NDE represents a biological paradox that challenges our understanding of the brain and has been advocated as evidence for life after death and for a noncorporeal basis of human consciousness, based on the unsupported belief that the brain cannot
possibly be the source of highly vivid and lucid conscious experiences during clinical death.
“By presenting evidence of highly organized brain activity and neurophysiologic features consistent with conscious processing at near-death, we now provide a scientific
framework to begin to explain the highly lucid and realer-than-real mental experiences reported by near-death survivors.”
The work of George Mashour, M.D., Ph.D., was supported by National Institutes of Health Grant and the James S. McDonnell Foundation.