Finally, an antibiotic that kills pathogens like MRSA without resistance
January 9, 2015
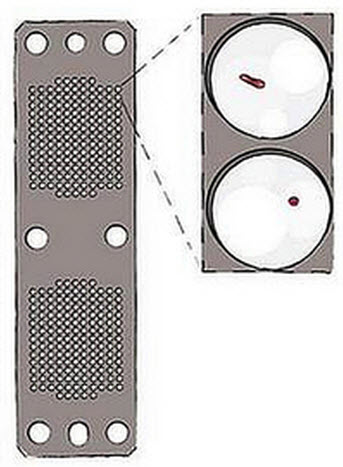
The iChip houses growing microorganisms, using semi-permeable membranes (shown as circles) on each side of the plate. After adding agar nutrient, it is placed in the soil from which the sample originated. (Credit: Losee L. Ling et al./Nature)
Northeastern University researchers have discovered an antibiotic called “teixobactin” that eliminates pathogens without encountering any detectable resistance — a finding that challenges long-held scientific beliefs and holds great promise for treating chronic infections like tuberculosis and those caused by MRSA.
Pathogens’ resistance to antibiotics is causing a public health crisis, according to Northwest’s University Distinguished Professor Kim Lewis.
Lewis’ lab played a key role in analyzing and testing teixobactin for resistance from pathogens. Lewis said this marks the first discovery of an antibiotic to which resistance by mutations of pathogens have not been identified.
The research was published Wednesday Jan. 7 in the journal Nature. Lewis and Northeastern biology professor Slava Epstein co-authored the paper with colleagues from the University of Bonn in Germany, NovoBiotic Pharmaceuticals in Cambridge, Massachusetts, and Selcia Limited in the United Kingdom.
Finally a solution for MRSA
The research team says teixobactin’s discovery presents a promising new opportunity to treat chronic infections caused by staphylococcus aureus (MRSA), the “superbug” that infects 1 million Americans annually and which is highly resistant to antibiotics; and tuberculosis, which requires a combination of therapies, with negative side effects.
The screening of soil microorganisms has produced most antibiotics, but only 1 percent of them will grow in the lab, and this limited resource was overmined in the 1960s, Lewis explained.
He and Epstein spent years seeking to address this problem by tapping into a new source of antibiotics beyond those created by synthetic means: uncultured bacteria, which can’t be grown in a petri dish and make up 99 percent of all species in external environments.
How to grow uncultured bacteria: resistance is futile
They developed a novel method for growing uncultured bacteria in their natural environment, which led to the founding of NovoBiotic. Their approach is based on the iChip, a miniature device Epstein’s team created that can isolate and help grow single cells in their natural environment, providing researchers with much improved access to uncultured bacteria. NovoBiotic has so far assembled about 50,000 strains of uncultured bacteria and discovered 25 new antibiotics, of which teixobactin is the latest and most interesting, Lewis said.
The antibiotic was discovered during a routine screening for antimicrobial material using this method. Lewis then tested the compound for resistance development and did not find mutant MRSA or Mycobacterium tuberculosis resistant to teixobactin, which was found to block several different targets in the cell wall synthesis pathway.
“Our impression is that nature produced a compound that evolved to be free of resistance,” Lewis said. “This challenges the dogma that we’ve operated under that bacteria will always develop resistance. Well, maybe not in this case.”
Going forward, the research team hopes to develop teixobactin into a drug.
In 2013, Lewis revealed groundbreaking research in a separate paper published by Nature that presented a novel approach to treat and eliminate MRSA: a way to destroy the dormant persister cells, which are key to the success of chronic infections caused by MRSA.
Lewis said this latest research lays new ground to advance his innovative work on treating MRSA and other chronic infections.
Abstract of A new antibiotic kills pathogens without detectable resistance
Antibiotic resistance is spreading faster than the introduction of new compounds into clinical practice, causing a public health crisis. Most antibiotics were produced by screening soil microorganisms, but this limited resource of cultivable bacteria was overmined by the 1960s. Synthetic approaches to produce antibiotics have been unable to replace this platform. Uncultured bacteria make up approximately 99% of all species in external environments, and are an untapped source of new antibiotics. We developed several methods to grow uncultured organisms by cultivation in situ or by using specific growth factors. Here we report a new antibiotic that we term teixobactin, discovered in a screen of uncultured bacteria. Teixobactin inhibits cell wall synthesis by binding to a highly conserved motif of lipid II (precursor of peptidoglycan) and lipid III (precursor of cell wall teichoic acid). We did not obtain any mutants of Staphylococcus aureus or Mycobacterium tuberculosis resistant to teixobactin. The properties of this compound suggest a path towards developing antibiotics that are likely to avoid development of resistance.