Functional brain imaging reliably predicts which vegetative patients have potential to recover consciousness
April 17, 2014
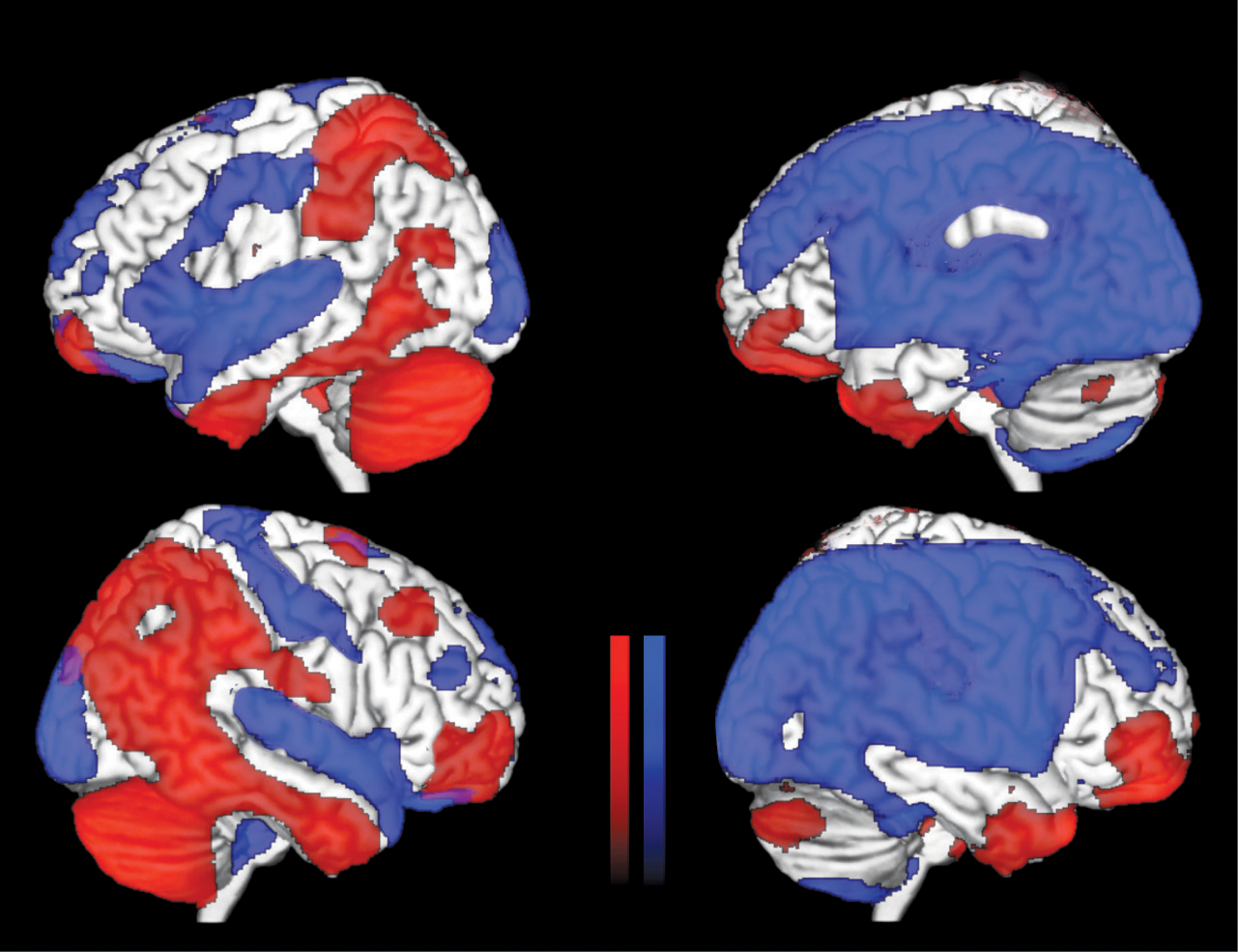
Statistical parametric mapping-analysis of fluorodeoxyglucose PET scans. Left: minimally conscious state; right: unresponsive wakefulness syndrome. Blue = areas with significantly lowered metabolism. Red = areas with preserved metabolism. (Credit: Johan Stender et al./The Lancet)
A functional brain imaging technique known as positron emission tomography (PET) is a promising tool for determining which severely brain damaged individuals in vegetative states have the potential to recover consciousness, according to new research published in The Lancet.
Surprisingly, this is the first time that researchers have tested the diagnostic accuracy of functional brain imaging techniques in clinical practice.
“Our findings suggest that PET imaging can reveal cognitive processes that aren’t visible through traditional bedside tests, and could substantially complement standard behavioral assessments to identify unresponsive or ‘vegetative’ patients who have the potential for long-term recovery,” says study leader Professor Steven Laureys from the University of Liége in Belgium.*
Misdiagnoses of level of consciousness
In severely brain-damaged individuals, judging the level of consciousness has proved challenging. Traditionally, bedside clinical examinations have been used to decide whether patients are in a minimally conscious state (MCS), in which there is some evidence of awareness and response to stimuli, or are in a vegetative state (VS) also known as unresponsive wakefulness syndrome, where there is neither, and the chance of recovery is much lower. But up to 40% of patients are misdiagnosed using these examinations.
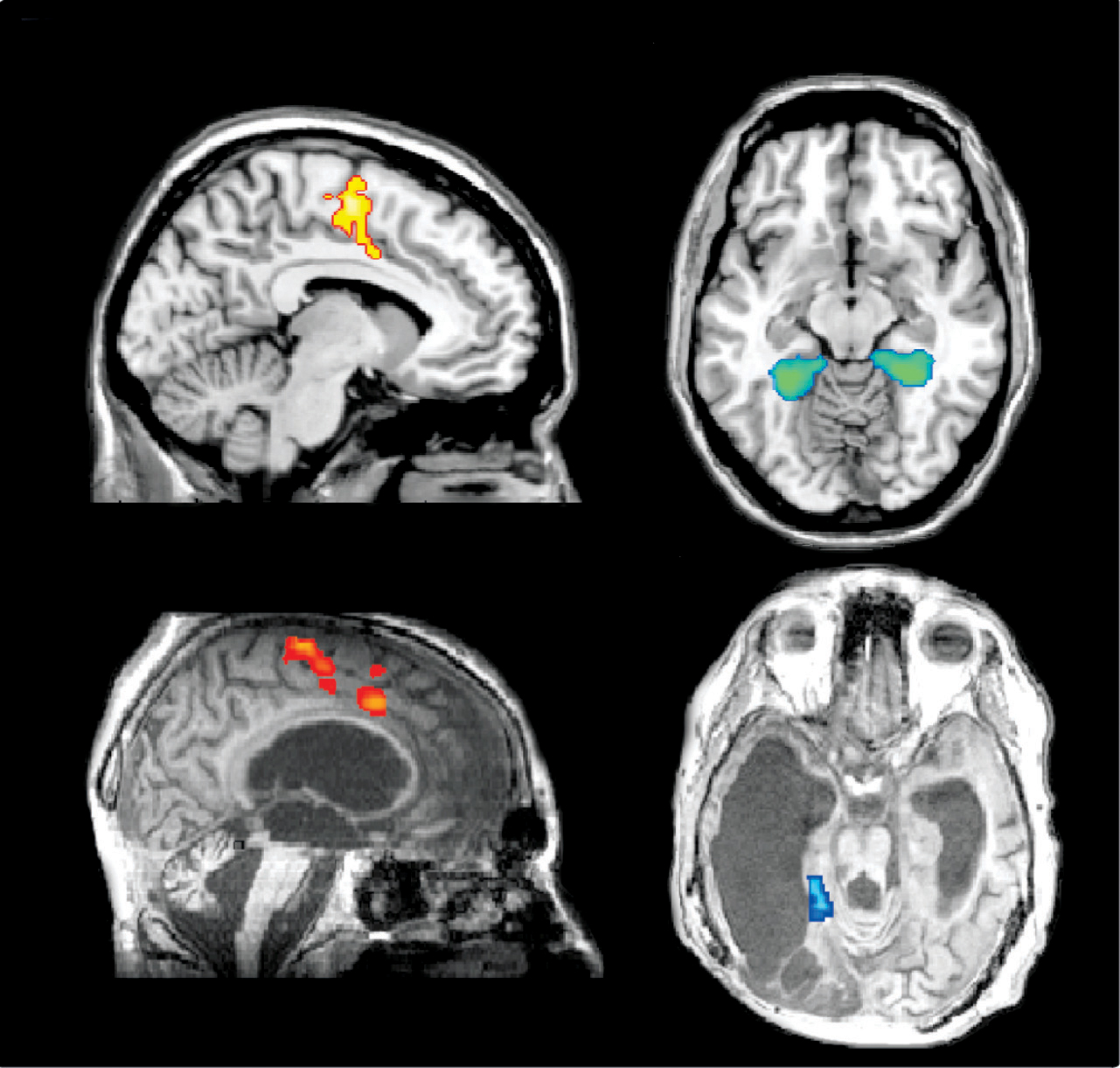
Functional MRI scans. Top: healthy control; bottom: patient with severe traumatic brain injury. Yellow and red = activations associated with motor imagery compared with spatial imagery tasks; blue and green = spatial imagery compared with motor imagery tasks. (Credit: Johan Stender et al./The Lancet)
“In patients with substantial cerebral edema [swelling of the brain], prediction of outcome on the basis of standard clinical examination and structural brain imaging is probably little better than flipping a coin,” writes Jamie Sleigh from the University of Auckland, New Zealand, and Catherine Warnaby from the University of Oxford, UK.
PET vs. fMRI
The study assessed whether two new functional brain imaging techniques — PET with the imaging agent fluorodeoxyglucose (FDG) and functional MRI (fMRI) during mental imagery tasks — could distinguish between vegetative and MCS in 126 patients with severe brain injury (81 in a MCS, 41 in a VS, and four with locked-in syndrome — a behaviorally unresponsive but conscious control group) referred to the University Hospital of Liége, in Belgium, from across Europe.
The researchers then compared their results with the well-established standardized Coma Recovery Scale–Revised (CSR-R) behavioural test, considered the most validated and sensitive method for discriminating very low awareness.
Overall, FDG-PET was better than fMRI in distinguishing conscious from unconscious patients. (Mental imagery fMRI was less sensitive at diagnosis of a MCS than FDG-PET (45% vs 93%), and had less agreement with behavioral CRS-R scores than FDG-PET (63% vs 85%). FDG-PET was about 74% accurate in predicting the extent of recovery within the next year, compared with 56% for fMRI.)
Importantly, a third of the 36 patients diagnosed as behaviorally unresponsive on the CSR-R test who were scanned with FDG-PET showed brain activity consistent with the presence of some consciousness. Nine patients in this group subsequently recovered a reasonable level of consciousness.
According to Professor Laureys, “We confirm that a small but substantial proportion of behaviorally unresponsive patients retain brain activity compatible with awareness. Repeated testing with the CRS–R complemented with a cerebral FDG-PET examination provides a simple and reliable diagnostic tool with high sensitivity towards unresponsive but aware patients. fMRI during mental tasks might complement the assessment with information about preserved cognitive capability, but should not be the main or sole diagnostic imaging method.”
The authors point out that the study was done in a specialist unit focusing on the diagnostic neuroimaging of disorders of consciousness, so getting it used in less specialist units might be more challenging.
Commenting on the study, Sleigh and Warnaby add, “From these data, it would be hard to sustain a confident diagnosis of unresponsive wakefulness syndrome solely on behavioral grounds, without PET imaging for confirmation…[This] work serves as a signpost for future studies. Functional brain imaging is expensive and technically challenging, but it will almost certainly become cheaper and easier. In the future, we will probably look back in amazement at how we were ever able to practice without it.”
Abstract of The Lancet paper
Background – Bedside clinical examinations can have high rates of misdiagnosis of unresponsive wakefulness syndrome (vegetative state) or minimally conscious state. The diagnostic and prognostic usefulness of neuroimaging-based approaches has not been established in a clinical setting. We did a validation study of two neuroimaging-based diagnostic methods: PET imaging and functional MRI (fMRI).
Methods – For this clinical validation study, we included patients referred to the University Hospital of Liège, Belgium, between January, 2008, and June, 2012, who were diagnosed by our unit with unresponsive wakefulness syndrome, locked-in syndrome, or minimally conscious state with traumatic or non-traumatic causes. We did repeated standardised clinical assessments with the Coma Recovery Scale—Revised (CRS—R), cerebral 18F-fluorodeoxyglucose (FDG) PET, and fMRI during mental activation tasks. We calculated the diagnostic accuracy of both imaging methods with CRS—R diagnosis as reference. We assessed outcome after 12 months with the Glasgow Outcome Scale—Extended.
Findings – We included 41 patients with unresponsive wakefulness syndrome, four with locked-in syndrome, and 81 in a minimally conscious state (48=traumatic, 78=non-traumatic; 110=chronic, 16=subacute). 18F-FDG PET had high sensitivity for identification of patients in a minimally conscious state (93%, 95% CI 85—98) and high congruence (85%, 77—90) with behavioural CRS—R scores. The active fMRI method was less sensitive at diagnosis of a minimally conscious state (45%, 30—61) and had lower overall congruence with behavioural scores (63%, 51—73) than PET imaging. 18F-FDG PET correctly predicted outcome in 75 of 102 patients (74%, 64—81), and fMRI in 36 of 65 patients (56%, 43—67). 13 of 42 (32%) of the behaviourally unresponsive patients (ie, diagnosed as unresponsive with CRS—R) showed brain activity compatible with (minimal) consciousness (ie, activity associated with consciousness, but diminished compared with fully conscious individuals) on at least one neuroimaging test; 69% of these (9 of 13) patients subsequently recovered consciousness.
Interpretation – Cerebral 18F-FDG PET could be used to complement bedside examinations and predict long-term recovery of patients with unresponsive wakefulness syndrome. Active fMRI might also be useful for differential diagnosis, but seems to be less accurate.
Funding – The Belgian National Funds for Scientific Research (FNRS), Fonds Léon Fredericq, the European Commission, the James McDonnell Foundation, the Mind Science Foundation, the French Speaking Community Concerted Research Action, the University of Copenhagen, and the University of Liège.