How to ‘switch off’ autoimmune diseases
September 8, 2014
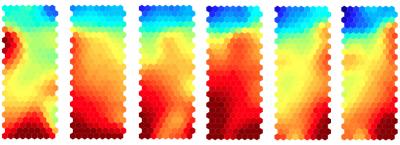
Aggressor cells, which have the potential to cause autoimmunity, are targeted by a treatment that causes conversion of these cells into protector cells. Gene expression changes gradually at each stage of treatment, as illustrated by the color changes in this series of heat maps. (Credit: University of Bristol/Dr. Bronwen Burton)
University of Bristol researchers have discovered how to stop cells from attacking healthy body tissue in debilitating autoimmune diseases (such as multiple sclerosis), where the body’s immune system destroys its own tissue by mistake.
The cells were converted from being aggressive to actually protecting against disease.
The study, funded by the Wellcome Trust, was published September 3 in Nature Communications (open access).
The researchers hope the finding will lead to widespread use of “antigen-specific immunotherapy” as a treatment for many autoimmune disorders, including multiple sclerosis (MS), type 1 diabetes, Graves’ disease, and systemic lupus erythematosus (SLE). (An antigen is a substance that generates an adaptive immune response.)
From aggressor to protector
Scientists were able to selectively target the cells that cause autoimmune disease by reducing their aggression against the body’s own tissues and converting them into cells capable of protecting against disease. This type of conversion has been previously applied to allergies (“allergic desensitization”). They also found that effective treatment is achieved by gradually increasing the dose of antigenic fragment injected.
To find out how this type of immunotherapy works, the scientists delved inside the immune cells themselves to see which genes and proteins were turned on or off by the treatment. They found changes in gene expression that help explain how effective treatment leads to conversion of aggressor into protector cells.
By specifically targeting the specific aggressor cells, this immunotherapeutic approach avoids the need for the immune suppressive drugs associated with infections, development of tumors, and disruption of natural regulatory mechanisms.
“Insight into the molecular basis of antigen-specific immunotherapy opens up exciting new opportunities to enhance the selectivity of the approach while providing valuable markers with which to measure effective treatment,” said Professor David Wraith, who led the research. “These findings have important implications for the many patients suffering from autoimmune conditions that are currently difficult to treat.”
MS affects around 100,000 people in the UK and 2.5 million people worldwide.
This treatment approach is currently undergoing clinical development through biotechnology company Apitope, a spinoff of the University of Bristol.
Abstract of Nature Communications paper
Antigen-specific immunotherapy combats autoimmunity or allergy by reinstating immunological tolerance to target antigens without compromising immune function. Optimization of dosing strategy is critical for effective modulation of pathogenic CD4+ T-cell activity. Here we report that dose escalation is imperative for safe, subcutaneous delivery of the high self-antigen doses required for effective tolerance induction and elicits anergic, interleukin (IL)-10-secreting regulatory CD4+ T cells. Analysis of the CD4+ T-cell transcriptome, at consecutive stages of escalating dose immunotherapy, reveals progressive suppression of transcripts positively regulating inflammatory effector function and repression of cell cycle pathways. We identify transcription factors, c-Maf and NFIL3, and negative co-stimulatory molecules, LAG-3, TIGIT, PD-1 and TIM-3, which characterize this regulatory CD4+ T-cell population and whose expression correlates with the immunoregulatory cytokine IL-10. These results provide a rationale for dose escalation in T-cell-directed immunotherapy and reveal novel immunological and transcriptional signatures as surrogate markers of successful immunotherapy.