Magnetic stimulation of the brain improves memory in schizophrenia
March 14, 2013
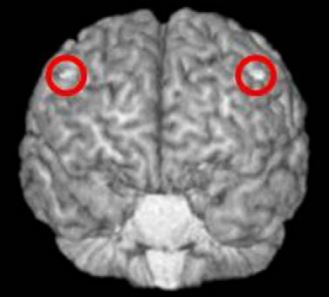
Targeting the dorsolateral prefrontal cortex for repetitive transcranial magnetic stimulation. (credit: Mera S. Barr et al./Biological Psychiatry)
University of Toronto scientists have found evidence that stimulating the brain using repetitive transcranial magnetic stimulation (rTMS) may be an effective strategy to improve cognitive function for patients with schizophrenia.
“In a randomized controlled trial, we evaluated whether rTMS can improve working memory in schizophrenia,” said Dr. Mera Barr and senior author Dr. Zafiris Daskalakis. “Our results showed that rTMS resulted in a significant improvement in working memory performance relative to baseline.”
Transcranial magnetic stimulation is a non-invasive procedure that uses magnetic fields to stimulate nerve cells. It does not require sedation or anesthesia and so patients remain awake, reclined in a chair, while treatment is administered through coils placed near the forehead.
“TMS can have lasting effects on brain circuit function because this approach not only changes the activity of the circuit that is being stimulated, but it also may change the plasticity of that circuit, i.e., the capacity of the circuit to remodel itself functionally and structurally to support cognitive functions,” explained Dr. John Krystal, Editor of Biological Psychiatry., where the scientists’ paper appears.
Previous work has shown that rTMS improves working memory in healthy individuals and a recent open-label trial showed promising findings for verbal memory in schizophrenia patients. This series of findings led this study to determine if high frequency rTMS could improve memory in individuals with schizophrenia.
They recruited medicated schizophrenia patients who completed a working memory task before and after 4 weeks of treatment. Importantly, this was a double-blind study, where neither the patients nor the researchers knew who was receiving real rTMS or a sham treatment that was designed to entirely mimic the procedure without actually delivering brain stimulation.
rTMS not only improved working memory in patients after 4 weeks, but the improvement was to a level comparable to healthy subjects. These findings suggest that rTMS may be a novel, efficacious, and safe treatment for working memory deficits in schizophrenia.
In 2008, rTMS was FDA-approved to treat depression for individuals who don’t respond to pharmacotherapy. The hope is that additional research will replicate these findings and finally provide an approved treatment for cognitive impairments in schizophrenia.