Magnetically levitated tissues could speed toxicity tests
January 29, 2013
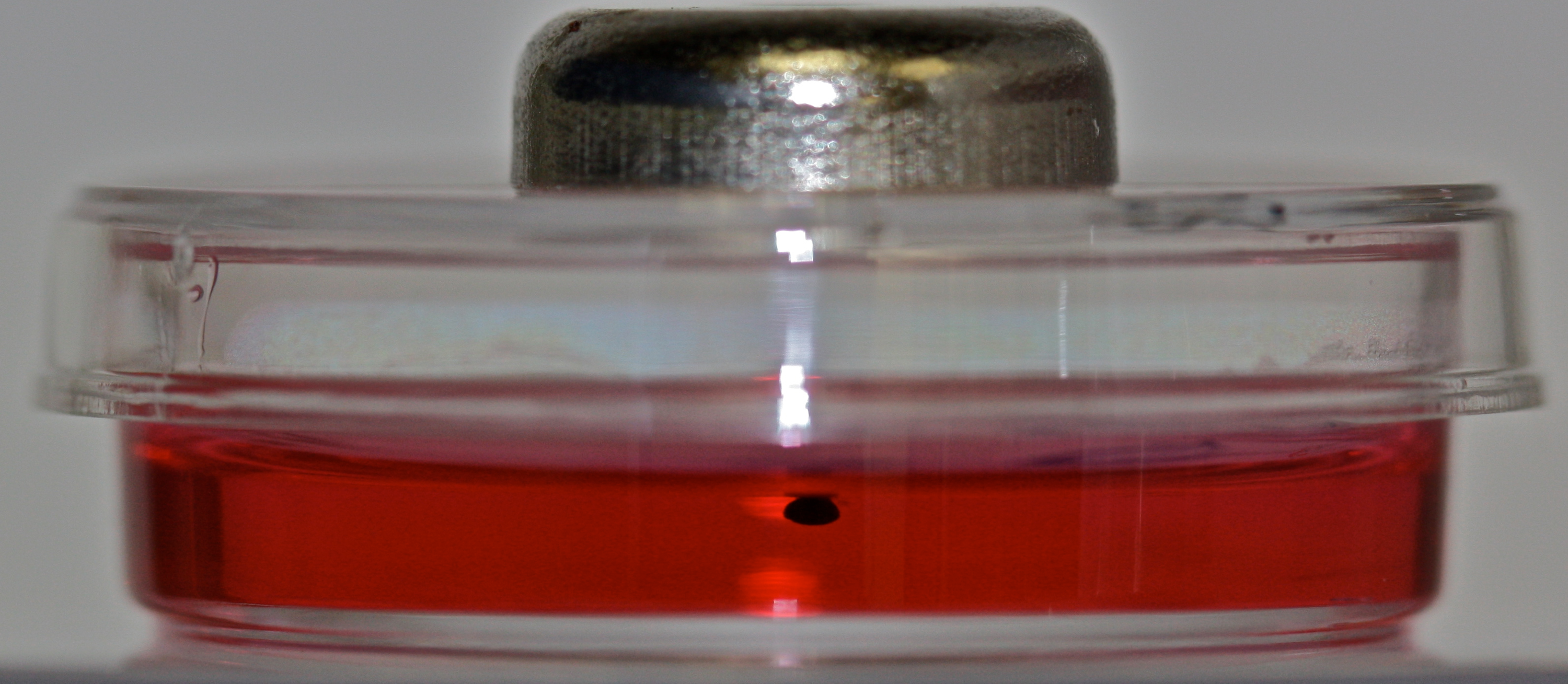
Rice University spinoff company Nano3D Biosciences uses magnetic levitation to grow three dimensional cell cultures. The technology uses inert, nontoxic nanoparticles and magnets to lift and suspend cells as they grow and divide. (Credit: Nano3D Biosciences)
In a development that could lead to faster and more effective toxicity tests for airborne chemicals, scientists from Rice University and the Rice spinoff company Nano3D Biosciences have used magnetic levitation to grow some of the most realistic lung tissue ever produced in a laboratory.
The research is part of an international trend in biomedical engineering to create laboratory techniques for growing tissues that are virtually identical to those found in people’s bodies.
In the new study, researchers combined four types of cells to replicate tissue from the wall of the bronchiole deep inside the lung.
Bronchials (credit: Wikimedia Commons)
“One of the unique things about the magnetic levitation technology is that it allows us to move cells around and arrange them the way that we want for a particular types of tissue,” said study co-author Tom Killian, professor and department chair of physics and astronomy at Rice.
From 2D to 3D cell cultures
“This is the first time anyone has arranged these four cell types in the same way that they are found in lung tissue.”
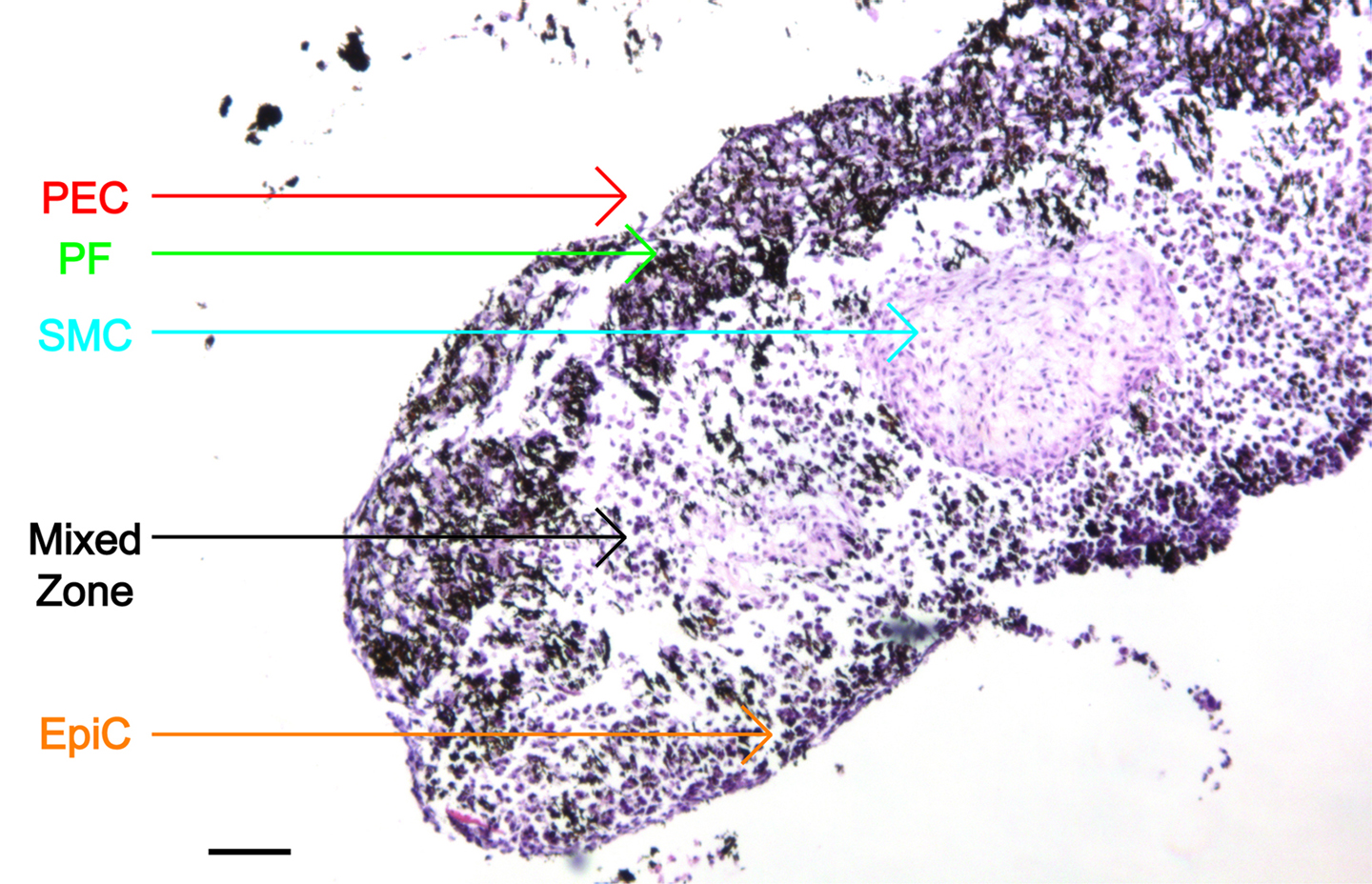
This microscopic image shows the structure and layers of in vitro bronchiole tissue created at Rice University and Nano3D Biosciences. The cell layers include epithelial cells (EpiC), smooth muscle cells (SMC), pulmonary fibroblasts (PF) and pulmonary endothelial cells (PEC). (Credit: Hubert Tseng/Rice University)
In vitro laboratory tests have historically been conducted on 2D cell cultures grown in flat petri dishes, but scientists have become increasingly aware that cells in flat cultures sometimes behave and interact differently than cells that are immersed in 3D tissue.
Killian and fellow scientists from Rice and the University of Texas MD Anderson Cancer Center co-founded Nano3D Biosciences in 2009 after creating a technology that uses magnetism to levitate and grow 3D cell cultures.
Magnetic nanoparticles
The technology relies on inert, nontoxic magnetic nanoparticles that are inserted into the living cells. Researchers can then use magnets to lift and suspend the cells as they grow and divide.
“Growing realistic lung tissues in vitro is a particular challenge,” said study co-author Jane Grande-Allen, professor of bioengineering at Rice. “There are a number of technical obstacles, and scientific funding agencies have placed a particular emphasis on lung tissue because there’s a large potential payoff in terms of reducing costs for pharmaceutical and toxicological testing.”
Nano3D Biosciences won a Small Business Innovation Research (SBIR) grant from the National Science Foundation (NSF) in 2011 to create a four-layered lung tissue from endothelial cells, smooth muscle cells, fibroblasts, and epithelial cells.

This composite shows 3D cultures of four types of cells that Rice University scientists combined in vitro to create bronchiole lung tissue. The cells are: epithelial cells (EpiC), smooth muscle cells (SMC), pulmonary fibroblasts (HPF) and pulmonary endothelial cells (PEC). (Credit: Hubert Tseng/Rice University)
A student team, Cells in 3-D, worked on a magnetic pen that could be used to grab, move and combine magnetized 3D cell cultures. It was used to create layered bronchiole tissues for this new study.
The researchers said the new tissue resembles native bronchiole tissue more closely than any other tissue yet created in the lab.
Realistic testing of airborne toxins
Glauco Souza, the company’s chief scientific officer, said bronchiole tissue could solve another problem that’s frequently encountered in testing the toxicity of airborne agents.
“With traditional 2-D cultures, it is very difficult to culture cells at the air-liquid interface, which is what you’d prefer for toxicity testing,” he said. “With our technology, we can easily levitate the bronchiole tissue to the air-liquid interface so that airborne toxins are exposed to the epithelial layer of the tissue, just as it would occur in the lungs.”
The researchers have already used the same methods pioneered in the bronchiole study to produce heart valve tissue. The NSF has awarded the company with a second phase of SBIR funding to further develop the technique for other types of tissue.
The research was funded by NSF and the Texas Emerging Technologies Fund.