Nanoparticles reboot blood flow in brain after injury
August 27, 2012
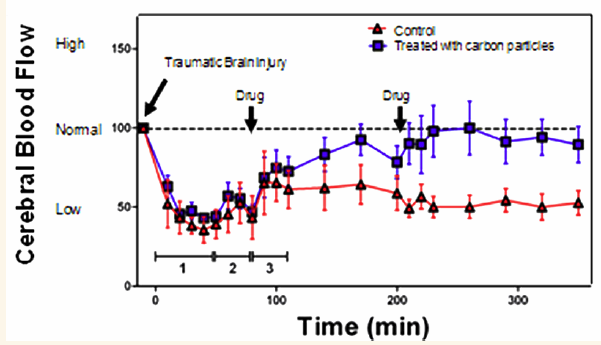
Polyethylene glycol-hydrophilic carbon clusters (PEG-HCCs) rapidly restore cerebral blood flow in a mild traumatic brain injury to a rat model (credit: Brittany R. Bitner et al./ACS Nano)
A nanoparticle developed at Rice University and tested in collaboration with Baylor College of Medicine (BCM) may bring great benefits to the emergency treatment of brain-injury victims, even those with mild injuries, including stroke.
“This might be a first line of defense against reactive oxygen species (ROS), which are always overstimulated during a medical trauma, whether that be to an accident victim or an injured soldier,” said Rice chemist and co-author James Tour, Rice’s T.T. and W.F. Chao Chair in Chemistry as well as a professor of mechanical engineering and materials science and of computer science. “They’re certainly exacerbated when there’s trauma with massive blood loss.”
Background: serious risks from brain injuries
In a traumatic brain injury, cells release an excessive amount of an ROS known as superoxide (SO) into the blood. Superoxides are toxic free radicals (molecules with one unpaired electron) that the immune system normally uses to kill invading microorganisms. Healthy organisms balance SO with superoxide dismutase (SOD), an enzyme that neutralizes it. But even mild brain trauma can release superoxides at levels that overwhelm the brain’s natural defenses.
“Superoxide is the most deleterious of the reactive oxygen species, as it’s the progenitor of many of the others,” Tour said. “If you don’t deal with SO, it forms peroxynitrite and hydrogen peroxide. SO is the upstream precursor to many of the downstream problems.”
SO affects the autoregulatory mechanism that manages the sensitive circulation system in the brain. Normally, vessels dilate when blood pressure is low and constrict when high to maintain an equilibrium, but a lack of regulation can lead to brain damage beyond what may have been caused by the initial trauma.
Combined polyethylene glycol-hydrophilic carbon clusters (PEG-HCC), which are already being tested to enhance cancer treatment, are also antioxidants. In animal studies, injections of PEG-HCC during initial treatment after an injury helped restore balance to the brain’s vascular system.
A PEG-HCC infusion that quickly stabilizes blood flow in the brain would be a significant advance for emergency care workers and battlefield medics, said Tour.
In tests, the researchers found PEG-HCC nanoparticles immediately and completely quenched superoxide activity and allowed the autoregulatory system to quickly regain its balance. Tour said ROS molecules readily combine with PEG-HCCs, generating “an innocuous carbon double bond, so it’s really radical annihilation. There’s no such mechanism in biology.”
While an SOD enzyme can alter only one superoxide molecule at a time, a single PEG-HCC about the size of a large protein at 2–3 nanometers wide and 30–40 nanometers long can quench hundreds or thousands.
“This is the most remarkably effective thing I’ve ever seen,” Kent said. “Literally within minutes of injecting it, the cerebral blood flow is back to normal, and we can keep it there with just a simple second injection. In the end, we’ve normalized the free radicals while preserving nitric oxide (which is essential to autoregulation). These particles showed the antioxidant mechanism we had previously identified as predictive of effectiveness.”
Kent said the nanoparticles as tested showed no signs of toxicity, but any remaining concerns should be answered by further tests. The researchers found the half-life of PEG-HCCs in the blood – the amount of time it takes for half the particles to leave the body – to be between two and three hours. Tests with different cell types in vitro showed no toxicity, he said.
The research has implications for stroke victims and organ transplant patients as well, Tour said.
The research was funded by the Department of Defense’s Mission Connect Mild Traumatic Brain Injury Consortium, the National Science Foundation, the National Institutes of Health and the National Heart, Lung and Blood Institute.