New MRI technique may predict rate of progress and prion-like spread of dementias
April 13, 2012
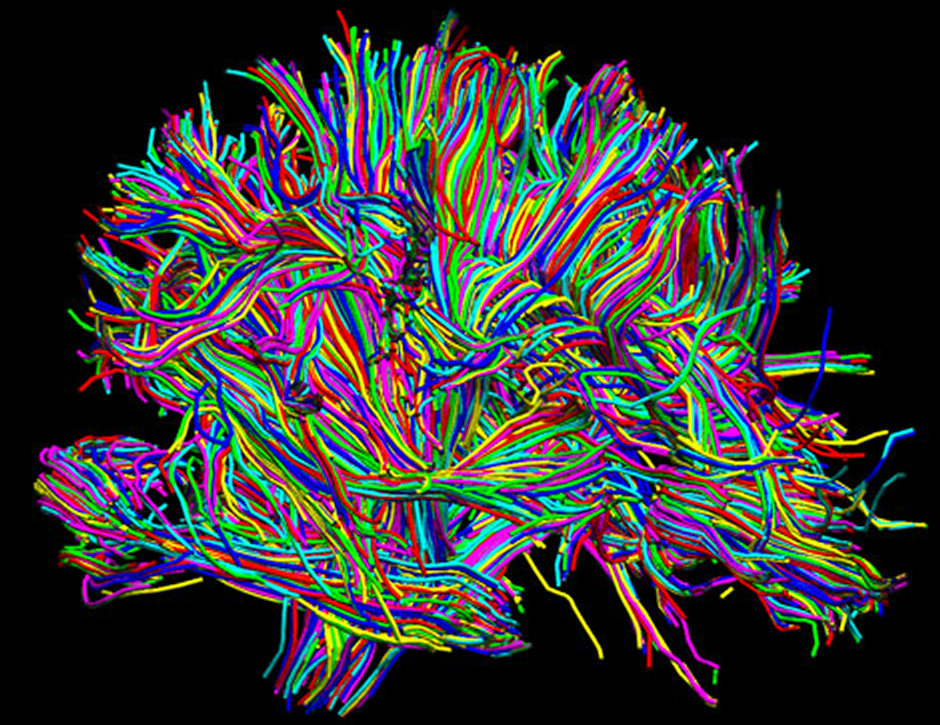
White matter connections in human brain (credit: David Shattuck, Arthur Toga, Paul Thompson/UCLA Lab of Neuro Imaging)
A new technique for analyzing brain images may make it possible to predict the rate of progression and physical path of many degenerative brain diseases, using just one magnetic resonance imaging (MRI) image, report scientists at the San Francisco VA Medical Center ( SFVAMC) and the University of California, San Francisco (UCSF).
The technique, developed by SFVAMC scientists in collaboration with a team led by Bruce Miller, MD, clinical director of the UCSF Memory and Aging Center, also supports mounting evidence that dementias spread through the brain along specific neuronal pathways in the same manner as prion diseases.
MRI images of brain degeneration
The scientists developed and used new computer modeling techniques to realistically predict the physical progression of Alzheimer’s disease and frontotemporal dementia (FTD), using images of 14 healthy brains. The models were based on whole-brain tractography, an MRI technique that maps the neural pathways, or “communication wires,” that connect different areas of the brain. The spread of disease along those pathways, as predicted by the models, closely matched actual MRI images of brain degeneration in 18 Alzheimer’s patients and 18 FTD patients.
“The results need to be replicated, but they suggest that by using this approach, we can predict the location and course of future brain atrophy in Alzheimer’s, FTD and other degenerative brain diseases, based on just one MRI taken at the outset of the disease,” said senior author Michael Weiner, MD, director of the SFVAMC Center for Imaging of Neurodegenerative Diseases. “This would be extremely useful in planning treatment, and in helping patients and families know what to expect as dementia progresses.”
Prion-like spread along networks in the brain
Weiner, who is also a UCSF professor of radiology, medicine, psychiatry and neurology, said that the results were “consistent with an emerging concept that brain damage occurs in these neurodegenerative diseases in a diffusive, prion-like propagation.”
A prion is an infectious, misfolded form of a normal protein. These proteins leave destructive amyloid deposits in the brains in which they develop, causing degeneration and eventual death. They are responsible for Creutzfeldt-Jakob disease in humans and bovine spongiform encephalopathy, or “mad cow” disease, in cattle. In 1997, neurologist Stanley B. Prusiner of UCSF was awarded the Nobel Prize in Medicine for discovering and characterizing the prion. His finding overturned a tenet of modern biology by showing that a protein, rather than just the molecules DNA and RNA, could cause infection.
“The idea of a prion-like mode of progression in dementias, which many scientists are beginning to support, is that the misfolded protein in one neuron will infect a neighboring brain cell, causing proteins in that cell to misfold in turn, and that the spread of these misfolded proteins flows along certain networks in the brain,” explained Weiner. “For instance, in Alzheimer’s, there is a spread of amyloid protein along the memory network. This paper reinforces the idea that the damage occurs progressively along that network and others.”
Weiner emphasized that Alzheimer’s and frontotemporal dementia “are not infectious diseases” like Creutzfeldt-Jakob. But he said “it may be that a little seed of the disease begins in one neuron in the brain and spreads in a similar way — so it’s infectious within the brain, from one neuron to the next.”
Ref.: Ashish Raj, Amy Kuceyeski, Michael Weiner, A Network Diffusion Model of Disease Progression in Dementia, Neuron, 2012; [DOI:10.1016/j.neuron.2011.12.040]