Scientists turn skin cells into neural precursors, bypassing stem-cell stage
February 1, 2012
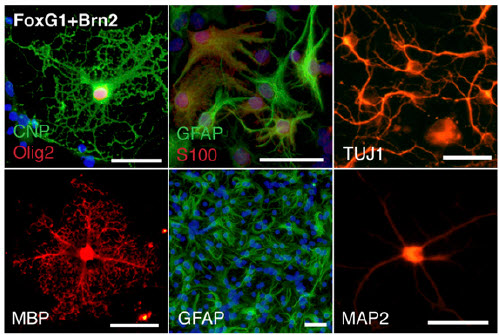
Neural precursor cells (upper left) differentiate into oligodendrocytes, astrocytes, and neurons (credit: Ernesto Lujana et al./PNAS)
Mouse skin cells can be converted directly into cells that become the three main parts of the nervous system, according to researchers at the Stanford University School of Medicine.
The finding is an extension of a previous study by the same group showing that mouse and human skin cells can be directly converted into functional neurons.
Neural precursor cells
This new study transforms the skin cells into neural precursor cells, as opposed to just neurons. They can also become the two other main cell types in the nervous system: astrocytes and oligodendrocytes.
Neural precursor cells offer another advantage over neurons:they can be cultivated to large numbers in the laboratory — a feature critical for their long-term usefulness in transplantation or drug screening. The finding implies that it may one day be possible to generate a variety of neural-system cells for transplantation that would perfectly match a human patient.
“We’ve shown the cells can integrate into a mouse brain and produce a missing protein important for the conduction of electrical signal by the neurons,” said Marius Wernig, MD, assistant professor of pathology and a member of Stanford’s Institute for Stem Cell Biology and Regenerative Medicine. “This is important because the mouse model we used mimics that of a human genetic brain disease. However, more work needs to be done to generate similar cells from human skin cells and assess their safety and efficacy.”
Bypassing induced pluripotency and embryonic stem cells
The multiple successes of the direct conversion method could refute the idea that pluripotency (a term that describes the ability of stem cells to become nearly any cell in the body) is necessary for a cell to transform from one cell type to another. Together, the results raise the possibility that embryonic stem cell research and another technique called “induced pluripotency” could be supplanted by a more direct way of generating specific types of cells for therapy or research.
Scientists had thought that it was necessary for a cell to first enter an induced pluripotent state or for researchers to start with an embryonic stem cell, which is pluripotent by nature, before it could go on to become a new cell type. However, research from Wernig’s laboratory in early 2010 showed that it was possible to directly convert one “adult” cell type to another with the application of specialized transcription factors, a process known as transdifferentiation.
“Dr. Wernig’s demonstration that fibroblasts can be converted into functional nerve cells opens the door to consider new ways to regenerate damaged neurons using cells surrounding the area of injury,” said pediatric cardiologist Deepak Srivastava, MD, who was not involved in these studies.
“It also suggests that we may be able to transdifferentiate cells into other cell types.” Srivastava is the director of cardiovascular research at the Gladstone Institutes at the University of California-San Francisco. In 2010, Srivastava transdifferentiated mouse heart fibroblasts into beating heart muscle cells.
“Direct conversion [from skin] has a number of advantages,” said Graduate student Ernesto Lujan, the first author. “It occurs with relatively high efficiency and it generates a fairly homogenous population of cells. In contrast, cells derived from iPS cells must be carefully screened to eliminate any remaining pluripotent cells or cells that can differentiate into different lineages.” Pluripotent cells can also cause cancers when transplanted into animals or humans, according to the scientists.
Human transplantation experiments
The scientists are now working to replicate the work with skin cells from adult mice and humans, but Lujan emphasized that much more research is needed before any human transplantation experiments could be conducted. In the meantime, however, the ability to quickly and efficiently generate neural precursor cells that can be grown in the laboratory to mass quantities and maintained over time will be valuable in disease and drug-targeting studies.
“In addition to direct therapeutic application, these cells may be very useful to study human diseases in a laboratory dish or even following transplantation into a developing rodent brain,” said Wernig.
Ref.: E. Lujan, et al., Direct conversion of mouse fibroblasts to self-renewing, tripotent neural precursor cells, Proceedings of the National Academy of Sciences, 2012; [DOI:10.1073/pnas.1121003109]