Skin layer grown from human stem cells could replace animals in drug and cosmetics testing
April 28, 2014
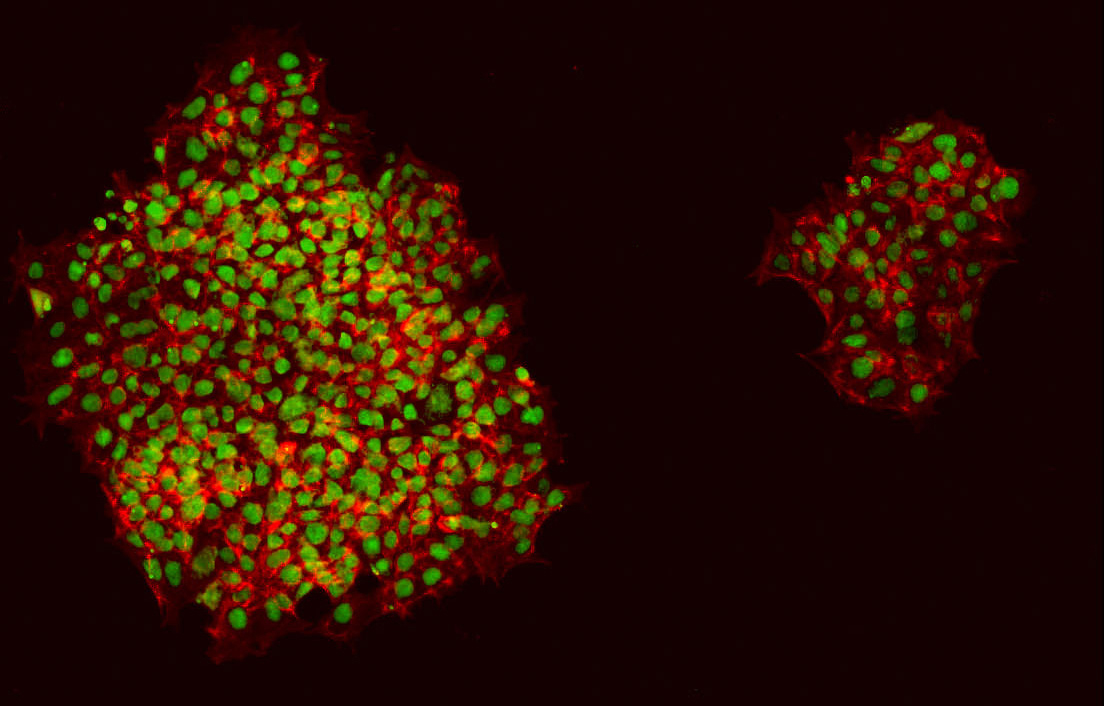
Keratinocyte (cells in the outermost layer of skin) colonies developed from human induced pluripotent stem cells (credit: King’s College London)
An international team led by King’s College London and the San Francisco Veteran Affairs Medical Center (SFVAMC) has developed the first lab-grown epidermis (the outermost skin layer) with a functional permeability barrier akin to real skin.
The new epidermis, grown from human pluripotent stem cells, offers a cost-effective alternative lab model for testing drugs and cosmetics, and could also help to develop new therapies for rare and common skin disorders.
The epidermis, the outermost layer of human skin, forms a protective interface between the body and its external environment, preventing water from escaping and microbes and toxins from entering.
Tissue engineers have been unable to grow epidermis with the functional barrier needed for drug testing or produce an in vitro (lab) model for large-scale drug screening. That’s because the number of cells that can be grown from a single skin biopsy sample has been limited.
The new study, published in the journal Stem Cell Reports (open access), describes the use of human induced pluripotent stem cells (iPSC) (stem cells that can develop into different types of body cells) to produce an unlimited supply of pure keratinocytes (the predominant cell type in the outermost layer of skin). These new keratinocytes closely match keratinocytes generated from other stem-cell types: human embryonic stem cells (hESC) and primary keratinocytes from skin biopsies.
Making artificial skin in the lab
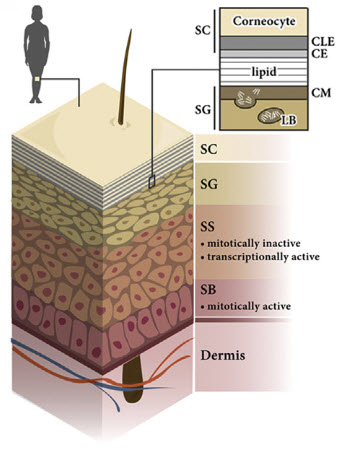
Schematic drawing of normal human skin, depicting the epidermal permeability barrier within the stratum corneum (the outermost layer of epidermis) (credit: Anastasia Petrova et al./Stem Cell Reports)
This supply of new keratinocytes was then used to manufacture 3D epidermal equivalents to build a functional permeability barrier, which in natural human skin is essential in protecting the body from losing moisture and preventing the entry of chemicals, toxins and microbes.
A comparison of epidermal equivalents generated from iPSC stem cells, hESC stem cells, and primary human keratinocytes (skin cells) from skin biopsies from the outermost layer of normal human skin showed no significant difference in their structural or functional properties.
“The ability to obtain an unlimited number of genetically identical units can be used to study a range of conditions where the skin’s barrier is defective due to mutations in genes involved in skin barrier formation, such as ichthyosis (dry, flaky skin) or atopic dermatitis,” said Theodora Mauro, leader of the SFVAMC team.
Studying disease effects and repair methods
“We can use this model to study how the skin barrier develops normally, how the barrier is impaired in different diseases, and how we can stimulate its repair and recovery.”
“Our new method can be used to grow much greater quantities of lab-grown human epidermal equivalents, and thus could be scaled up for commercial testing of drugs and cosmetics,” said Dusko Ilic, leader of the team at King’s College London.
“Human epidermal equivalents representing different types of skin could also be grown, depending on the source of the stem cells used, and could thus be tailored to study a range of skin conditions and sensitivities in different populations.”
Abstract of Stem Cell Reports paper
- Manufacture of HEEs with a functional epidermal barrier in vitro from hESCs/iPSCs
- Unique model for skin diseases with defective epidermal permeability barriers
- Easily adaptable model for use in regenerative and aesthetic medicine
- Cost-effective model for testing new drugs and cosmetics
Cornification and epidermal barrier defects are associated with a number of clinically diverse skin disorders. However, a suitable in vitro model for studying normal barrier function and barrier defects is still lacking. Here, we demonstrate the generation of human epidermal equivalents (HEEs) from human embryonic stem cells (hESCs) and induced pluripotent stem cells (iPSCs). HEEs are structurally similar to native epidermis, with a functional permeability barrier. We exposed a pure population of hESC/iPSC-derived keratinocytes, whose transcriptome corresponds to the gene signature of normal primary human keratinocytes (NHKs), to a sequential high-to-low humidity environment in an air/liquid interface culture. The resulting HEEs had all of the cellular strata of the human epidermis, with skin barrier properties similar to those of normal skin. Such HEEs generated from disease-specific iPSCs will be an invaluable tool not only for dissecting molecular mechanisms that lead to epidermal barrier defects but also for drug development and screening.