Smarter, cheaper technologies for improved point-of-care medicine in remote areas
May 8, 2015
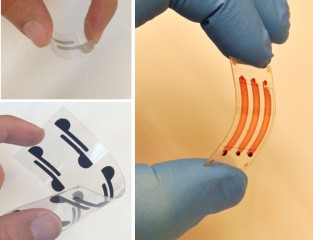
Flexible microchip with electrodes sends an electrical signal when patient samples contain HIV (credit: Shafiee, H. et al./ Scientific Reports
Stanford University School of Medicine scientists have developed new paper and flexible polymer substrates with special sensing devices for rapid and accurate detection of pathogens such as HIV, various bacteria, and CD4+ T lymphocytes.
These novel technologies offer the type of robust, simple, and inexpensive biosensing systems required to provide point-of-care health care in remote areas, where there is minimal diagnostic infrastructure or equipment and a lack of trained medical technicians.
Testing for HIV-1 in whole blood
Current tests for HIV infection detect antibodies to HIV in the individual’s blood but it takes up to several months for those antibodies to form, so those tests do not detect individuals in the earliest stage of infection when they are most likely to pass on the disease. To detect HIV-1 in recently infected individuals, the researchers developed a disposable flexible polyester chip with implanted electrodes.
HIV-1 antibodies are added to whole blood or plasma where they bind to the virus creating aggregates of antibody and viral lysate. When added to the flexible chip, the aggregates change the electrical conductivity of the chip, which gives a simple electrical readout indicating that the sample contains HIV-1.
In addition to detecting early stage infection, the electrical readout is much simpler and less expensive than current assays. The researchers estimate that the cost is about $2 per test and can be safely disposed of after use.
CD4+ T Lymphocyte capture and detection
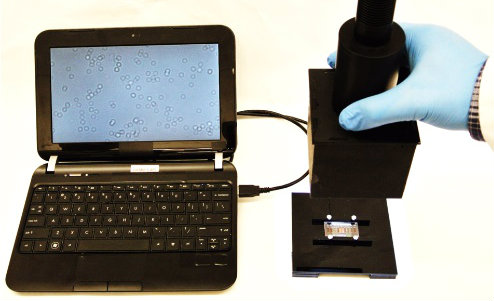
CD4+ T cells captured on the polyester film-based platform are imaged with the lensless device and are visible on the attached portable laptop screen (credit: Shafiee, H. et al./ Scientific Reports)
Accurate CD4+ T cell count is essential for HIV-1 diagnosis and treatment monitoring. World Health Organization guidelines recommend antiretroviral therapy for individuals with a CD4+ T cell count of less than 500 cells/ml.
Conventional CD4+ T cell counting methods require an expensive flow cytometer, a skilled operator, and costly reagents.
The research team developed a simple, inexpensive assay for CD4+ T cell count using two novel technologies: a polyester film with microfluidic channels to capture the T cells, and a detection technology known as lensless shadow imaging.
The microfluidic channels were coated with an antibody that captures the CD4+ T cells. A single drop of whole blood from a fingerprick was applied to the polyester film, where capillary forces pull the blood into the microfluidic channels. The shadow of the CD4+ T cells that adhere to the channels can then be visualized on the polyester film.
The platform allows efficient CD4+ T cell counting using fingerprick volume of unprocessed whole blood samples on disposable film at the point-of-care. This platform has the potential to replace the current use of non-disposable glass platforms that require additional steps and expense to visualize the cells with a fluorescent tag.
Using a cell phone to detect and quantify bacteria
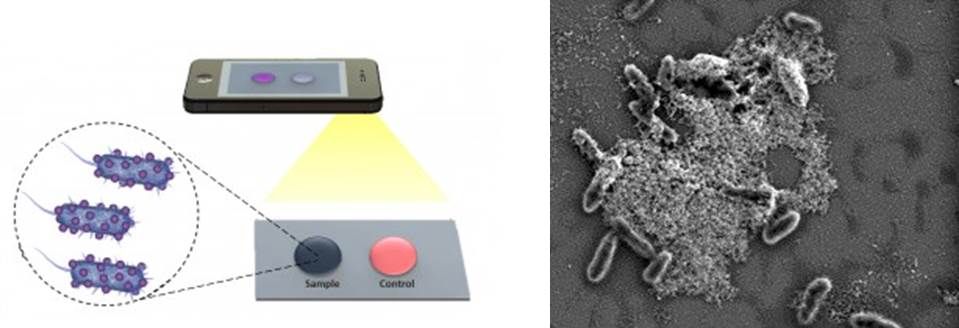
Left: Nanoparticles aggregate bacteria in a patient sample. The aggregation causes the sample to turn blue in contrast to the control, which is red. The cell phone photograph is used to determine the concentration of bacteria in the patient sample. Right: Scanning electron micrograph showing bacteria adhered to the gold nanoparticles on the substrate. (credit: Shafiee, H. et al./ Scientific Reports)
The researchers developed a sensitive biosensing platform that detects E. coli that bind to gold nanoparticles on cellulose paper. E. coli and S. aureus are the most common bacterial pathogens that cause food poisoning, skin infections, and blood infections.
When the test fluid containing bacteria is mixed with the nanoparticles and transferred to the cellulose paper, the aggregation results in a blue spot. If bacteria are not present, there is no aggregation and the solution applied to the cellulose paper turns red. So the presence or absence of bacteria can be seen immediately.
To determine the concentration of E.coli in the sample, the researchers took a picture of the blue spot on the paper with a cell phone and used an imaging analysis tool to measure red pixel intensity of the picture. Concentrations of E. coli could be quantified ranging from 8 to 1.5 million bacteria per milliliter. The platform can also be applied to other bacteria such as S. aureus.
“The goal of our work,” says Utkan Demirici, PhD., of the Demirici Bio-Acoustic-MEMS in Medicine Laboratory at Stanford School of Medicine, “is to simplify the techniques that both capture the biotarget and detect that captured target. Both aspects of a simplified test must be addressed to move this type of work forward to practical use in low resource settings.
“These platform technologies can be potentially broadly applied to other diseases, such as detecting oncogenic viruses such as KSHV, HPV, HBV and HCV, which we also need to be monitored in the developed world settings at a primary care physicians office, or during a dental appointment, or at the bedside. ”
Their research was reported in the March 6 edition of the open-access Nature Scientific Reports. It was funded in part by the National Institutes of Health through a grant from the National Institute of Biomedical Imaging and Bioengineering (NIBIB) and grants from the National Institute of Allergy and Infectious Diseases (NIAID) and the National Institute of General Medical Sciences (NIGMS).
Abstract of Paper and Flexible Substrates as Materials for Biosensing Platforms to Detect Multiple Biotargets
The need for sensitive, robust, portable, and inexpensive biosensing platforms is of significant interest in clinical applications for disease diagnosis and treatment monitoring at the point-of-care (POC) settings. Rapid, accurate POC diagnostic assays play a crucial role in developing countries, where there are limited laboratory infrastructure, trained personnel, and financial support. However, current diagnostic assays commonly require long assay time, sophisticated infrastructure and expensive reagents that are not compatible with resource-constrained settings. Although paper and flexible material-based platform technologies provide alternative approaches to develop POC diagnostic assays for broad applications in medicine, they have technical challenges integrating to different detection modalities. Here, we address the limited capability of current paper and flexible material-based platforms by integrating cellulose paper and flexible polyester films as diagnostic biosensing materials with various detection modalities through the development and validation of new widely applicable electrical and optical sensing mechanisms using antibodies and peptides. By incorporating these different detection modalities, we present selective and accurate capture and detection of multiple biotargets including viruses (Human Immunodeficieny Virus-1), bacteria (Escherichia coli and Staphylococcus aureus), and cells (CD4+ T lymphocytes) from fingerprick volume equivalent of multiple biological specimens such as whole blood, plasma, and peritoneal dialysis effluent with clinically relevant detection and sensitivity.