Taking tissue regeneration beyond the state-of-the-art
July 10, 2012
The University of Nottingham has begun the search for a new class of injectable materials that will stimulate stem cells to regenerate damaged tissue in degenerative and age-related disorders of the bone, muscle and heart.
The research could lead to treatments for diseases that currently have no cure. The aim is to produce radical new treatments that will reduce the need for invasive surgery, optimize recovery and reduce the risk of undesirable scar tissue.
The demand for organ transplants is great, but there are few donors and transplant rejection remains an ever present concern. This has led to the development of an interdisciplinary research field called “regenerative medicine.” Researchers within this field are not only looking to help patients requiring organ transplants, but also those with severe burns, muscle injuries, cardiovascular problems or patients with broken bones that are not healing.
The body’s wound repair process works in much the same way regardless of what the condition is or which organ is affected. For instance; the sequence of events that follows a heart attack is similar to the process that takes place following spinal-cord injury. The aim of regenerative medicine is to create a ‘seed bed’ from which tissue can grow. This technique will lead to more effective and affordable treatments for diseases such as cancer and osteoporosis and for patients who have suffered a heart attack or experienced major trauma.
Nanotechnology for drug delivery
Nottingham and UNMC are developing a new class of injectable material that stimulates stem cells to form new blood vessels, heart and bone tissue.
The research is part of the Rational Bioactive Materials Design for Tissue Generation project (Biodesign), a €11m EU-funded research project that involves 21 research teams from across Europe, made up of leading experts in degenerative disease and regenerative medicine.
“This research heralds a step-change in approaches to tissue regeneration,” said Kevin Shakesheff, Professor of Advanced Drug Delivery and Tissue Engineering and Head of the School of Pharmacy. “Current biomaterials are poorly suited to the needs of tissue engineering and regenerative medicine.
“The aim of Biodesign is to develop new materials and medicines that will stimulate tissue regeneration rather than wait for the body to start the process itself. The aim is to fabricate advanced biomaterials that match the basic structure of each tissue so the cells can take over the recovery process themselves.”
UNMC is building on its expertise in nanotechnology for drug delivery. “Our understanding of genomics and tissue regeneration means that medicines of the future will be much smarter,” said Dr Andrew Morris, an expert in transdermal drug delivery at UNMC. “We are moving away from simple drugs being given to a patient in a tablet and hoping that they will have the desired effect.
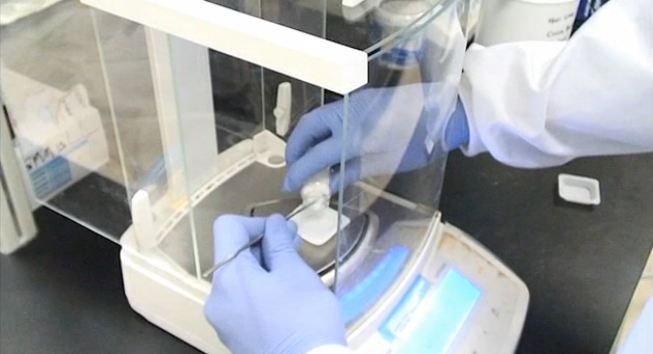
“Here in Malaysia we are looking at synthesizing microparticles which can potentially be injected directly into a patient at the site of injury to promote tissue re-growth. These microparticles would act as a scaffold to encourage regrowth in bone tissue, skeletal muscle and potentially even cardiac muscle.”