Virus-derived particles target blood cancer
August 15, 2013
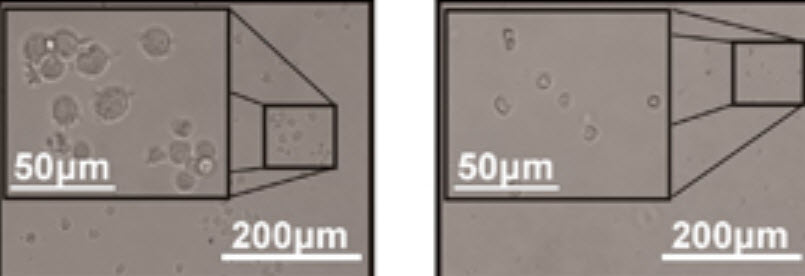
Brightfield microscopy images of leukemia patient samples treated with control saline (left) and NRRPs (right).
Ottawa researchers have developed unique virus-derived particles that can kill human blood cancer cells in the laboratory and eradicate the disease in mice, with few side effects.
The study is published in Blood Cancer Journal (open access) by co-senior authors Drs. David Conrad and John Bell of the Ottawa Hospital Research Institute (OHRI) and the University of Ottawa (uOttawa).
Bell and his colleagues have been investigating replicating viruses for the treatment of solid cancers for many years, with very promising results, but this is the first major success they have had treating blood cancer (leukemia). It is also the first success they have had using a non-replicating virus-derived particle (NRRP) as opposed to a replicating virus.
This time-lapse photography, taken over a 48-hour period, shows leukemia cells being attacked by the virus-derived particles. The cell membranes collapse as the leukemia cells die. Video courtesy David Conrad, Cory Batenchuk and Fabrice Le Boeuf, Ottawa Hospital Research Institute
‘Safe at high doses’
“Our research indicated that a replicating virus might not be the safest or most effective approach for treating leukemia, so we decided to investigate whether we could make virus-derived particles that no longer replicate but still kill cancer,” said Dr. Conrad, a hematologist conducting research in the Blood and Marrow Transplant Program at The Ottawa Hospital.
“We were delighted to see that this novel therapy was very safe at high doses, and worked extremely well in our laboratory leukemia models. We hope to test this in patients in the near future.”
The researchers used a specific method and dose of UV light to transform regular replicating viruses into unique particles that could no longer replicate and spread, but could still enter cancer cells efficiently, kill them and stimulate a strong immune response against the cancer.
These particles were able to kill multiple forms of leukemia in the laboratory, including samples taken from local patients who had failed all other therapies. Normal blood cells were not affected.
Sixty percent of mouse models of leukemia cured
This novel treatment was also successful in mouse models of leukemia. In fact, 80 per cent of the mice that received the therapy had markedly prolonged survival and 60 per cent were eventually cured, while all of the untreated mice died of their leukemia within 20 days.
“Leukemia is a devastating disease that can be very difficult to treat, and new therapies are urgently needed,” said Conrad. “While we’re still at the early stages of this research, I think this therapy holds a lot of promise because it appears to have a potent, long-lasting effect on leukemia without the debilitating side effects of many cancer therapies used in the clinic right now. We will likely see even better results once we optimize the dose in our preparations to advance this research into human clinical trials.”
This research was funded by the Ontario Institute for Cancer Research, the Terry Fox Foundation, the Natural Sciences and Engineering Research Council of Canada, the Canadian Institutes of Health Research, Ottawa’s Department of Medicine and The Ottawa Hospital Foundation.
Microfluidic chip for capturing live circulating tumor cells
In related news, researchers in China have developed a new microfluidic chip that can quickly and efficiently segregate and capture live circulating tumor cells (CTCs) from a patient’s blood, with potential applications for cancer screenings and treatment assessments.
Many currently available devices for detecting CTCs in patients’ blood are either too slow for clinical use or have other problems, such as a reduced ability to distinguish between the rare CTCs and more common white blood cells and other non-tumor cells, the researchers say.
The new system captures more than 90 percent of the CTCs, which makes it highly efficient. Overall processing time has also been shortened, thanks in part to a step in which red blood cells are selectively lysed, or broken apart. Lysing the red blood cells diminishes the tendency of blood to clog the system, a common problem that slows processing time in similar CTC filtering devices.
The ability to count live, individual CTCs in the bloodstream can help doctors determine the severity of a cancer, since CTC density in the blood is linked to the progression of the disease and patients’ likelihood of survival. The new method could also improve “liquid biopsy” techniques, in which a small amount of blood is drawn as an alternative to conventional tissue biopsies of primary or metastatic tumors.
In addition to potentially improving screening tests, the team believes their approach may someday help doctors control CTC-induced metastasis, which the researchers say can be far more lethal than the original tumor.
“Because our chip is able to capture viable CTCs, it creates opportunities for the development of new and efficient cancer biomarkers,” says co-author Ray Han, a professor at Peking University in Beijing.
The authors of the study are affiliated with Peking University, the National Center for Nanoscience and Technology in China and Chinese PLA General Hospital in Beijing.