Decoding nervous-system signals to the brain could speed up diagnosis of infections or inflammation
November 28, 2014
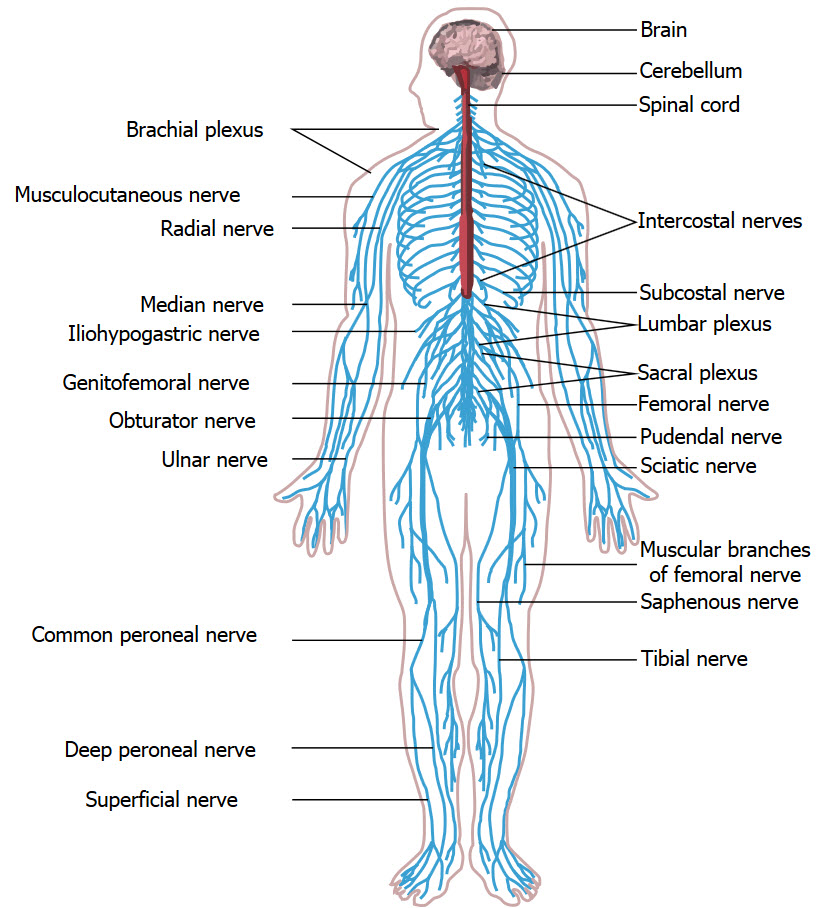
Peripheral nervous system (credit: Wikimedia Commons)
In a commentary published Thursday (Nov. 27) in the New England Journal of Medicine, researchers reviewed new pre-clinical trials that show that the nervous system may play a bigger role in infections and inflammation than previously known.
The researchers, at St. Michael’s Hospital in Toronto and the Feinstein Institute for Medical Research in Manhasset, NY, noted that neurons of the peripheral nervous system are known to send information about local infections or inflammation to the central nervous system (the brain and spinal cord), enabling the CNS to coordinate a whole-body response.
Benjamin Steinberg, M.D., a post-doctoral fellow and an anesthesiology resident at St. Michael’s, hypothesized that the neurons may be sending the CNS not just a general “danger warning” but specific information about whether the infection is caused by a virus or bacteria, the type of bacteria present, or the nature of the auto-immune reaction. Researchers are now trying to decipher that “neural code.”
Decoding the messages
“If we know the language and can read the code, in theory we can engineer or write our own,” said Steinberg, writing with coauthors Dr. Arthur Slutsky, vice-president of research at St. Michael’s and Dr. Kevin Tracey, president of the Feinstein Institute.
Since those messages are being sent from neurons to the CNS in real time, knowing what they’re “saying” could speed diagnoses or prognostication, which would be especially important in pandemics or outbreaks of particularly contagious or deadly diseases, such as flu, Ebola, or SARS.
The current method for confirming infections is to test body fluids or tissues, sometimes using invasive techniques, a process that can take hours, days or even longer. Steinberg also said researchers might even be able to tell how severe an infection is and how the illness is expected to progress without treatment.
“For example, we could perhaps tell quickly whether someone has the flu virus or bacterial pneumonia, which would determine whether antibiotics would be appropriate. At the extreme, a patient in septic shock requires prompt administration of antibiotic agents since each hour of delay is associated with a 7.6 per cent increase in mortality, but physicians do not always know what bacterium they need to target. An inappropriately chosen antibiotic can have serious ramifications for patient well-being.”
It’s already possible to intercept and even change some messages being sent to the CNS using bioelectric therapy. When injured, pain receptors send messages to the CNS that are registered as pain. Bioelectric therapy relieves pain by interrupting pain signals before they reach the brain. It also prompts the body to produce endorphins, which help to relieve pain.
In a related finding, stress signals from the body can trigger immune cells in the brain that can cause changes to the brain, resulting in mental disorders, as KurzweilAI reported Thursday.