Engineering new bone growth with coated tissue scaffolds
August 21, 2014
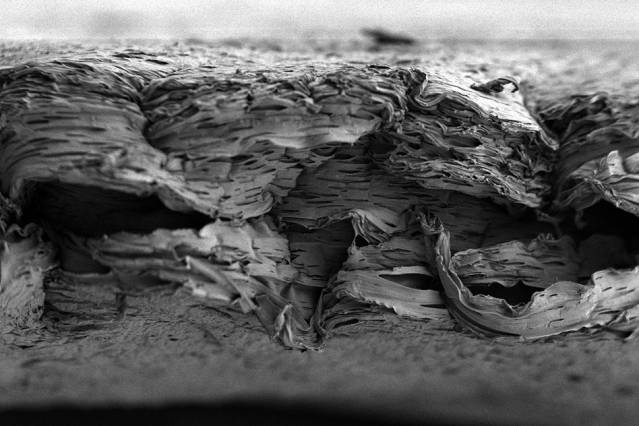
A scanning electron micrograph of a porous, nanostructured poly(lactic-co-glycolic acid) (PLGA) membrane. The membrane is coated with a polyelectrolyte (PEM) multilayer coating that releases growth factors to promote bone repair. (Credit: Nasim Hyder and Nisarg J. Shah)
MIT chemical engineers have devised a new treatment for bone injuries or defects: an implantable tissue scaffold (structure) coated with bone-growth factors that can be released slowly over a few weeks to induce the body to rapidly form new bone that looks and behaves just like the original tissue.
On Monday this week, KurzweilAI described a shape-memory polymer that expands with warm salt water to precisely fill bone defects and also acts as a scaffold for new bone growth.
The new method takes a different approach, using natural bone-growth factors. It could offer a dramatic improvement over the current standard for treating bone injuries: transplanting bone from another part of the patient’s body — a painful process that does not always supply enough bone, the engineers say.
Patients who could benefit include those with severe bone injuries (such as soldiers wounded in battle), those who suffer from congenital bone defects (such as craniomaxillofacial disorders), and those in need of bone augmentation before insertion of dental implants.
Stimulating bone growth with natural factors
Two of the most important natural bone growth factors are platelet-derived growth factor (PDGF) and bone morphogenetic protein 2 (BMP-2). As part of the natural wound-healing cascade, PDGF is one of the first factors released immediately following a bone injury, such as a fracture. After PDGF appears, other factors, including BMP-2, help to create the right environment for bone regeneration by recruiting cells that can produce bone and forming a supportive structure, including blood vessels.
Bu these are hard to deliver in a controlled manner, the engineers say. When very large quantities of growth factors are delivered too quickly, they are rapidly cleared from the treatment site — so they have reduced impact on tissue repair, and can also induce unwanted side effects.
“You want the growth factor to be released very slowly and with nanogram or microgram quantities, not milligram quantities,” says Paula Hammond, the David H. Koch Professor in Engineering and a member of MIT’s Koch Institute for Integrative Cancer Research and Department of Chemical Engineering. Hammond is the senior author of a paper on the research that appears in the Proceedings of the National Academy of Sciences.
“You want to recruit these native adult stem cells we have in our bone marrow to go to the site of injury and then generate bone around the scaffold, and you want to generate a vascular system to go with it.” This process takes time, so ideally the growth factors would be released slowly over several days or weeks.
To achieve this, the MIT team created a very thin, porous scaffold sheet coated with layers of PDGF and BMP. Using a technique called layer-by-layer assembly, they first coated the sheet with about 40 layers of BMP-2; on top of that are another 40 layers of PDGF. This allowed PDGF to be released more quickly, along with a more sustained BMP-2 release, mimicking aspects of natural healing.
“This is a major advantage for tissue engineering for bones because the release of the signaling proteins has to be slow and it has to be scheduled,” says Nicholas Kotov, a professor of chemical engineering at the University of Michigan who was not part of the research team.
The scaffold sheet is about 0.1 millimeter thick; once the growth-factor coatings are applied, scaffolds can be cut from the sheet on demand, and in the appropriate size for implantation into a bone injury or defect.
Effective repair
The researchers tested the scaffold in rats with a skull defect large enough — 8 millimeters in diameter — that it could not heal on its own. After the scaffold was implanted, growth factors were released at different rates. PDGF, released during the first few days after implantation, helped initiate the wound-healing cascade and mobilize different precursor cells to the site of the wound. These cells are responsible for forming new tissue, including blood vessels, supportive vascular structures, and bone.
BMP, released more slowly, then induced some of these immature cells to become osteoblasts, which produce bone. When both growth factors were used together, these cells generated a layer of bone, as soon as two weeks after surgery, that was indistinguishable from natural bone in its appearance and mechanical properties, the researchers say.
“Using this combination allows us to not only have accelerated proliferation first, but also facilitates laying down some vascular tissue, which provides a route for both the stem cells and the precursor osteoblasts and other players to get in and do their jobs. You end up with a very uniform healed system,” Hammond says.
Another advantage of this approach is that the scaffold is biodegradable and breaks down inside the body within a few weeks. The scaffold material, a polymer called PLGA, is widely used in medical treatment and can be tuned to disintegrate at a specific rate so the researchers can design it to last only as long as needed.
Hammond’s team has filed a patent based on this work and now aims to begin testing the system in larger animals in hopes of eventually moving it into clinical trials.
Other authors include members of the Harvard School of Dental Medicine and Brigham and Women’s Hospital. This study was funded by the National Institutes of Health.
Abstract of Proceedings of the National Academy of Sciences paper
Traumatic wounds and congenital defects that require large-scale bone tissue repair have few successful clinical therapies, particularly for craniomaxillofacial defects. Although bioactive materials have demonstrated alternative approaches to tissue repair, an optimized materials system for reproducible, safe, and targeted repair remains elusive. We hypothesized that controlled, rapid bone formation in large, critical-size defects could be induced by simultaneously delivering multiple biological growth factors to the site of the wound. Here, we report an approach for bone repair using a polyelectrolye multilayer coating carrying as little as 200 ng of bone morphogenetic protein-2 and platelet-derived growth factor-BB that were eluted over readily adapted time scales to induce rapid bone repair. Based on electrostatic interactions between the polymer multilayers and growth factors alone, we sustained mitogenic and osteogenic signals with these growth factors in an easily tunable and controlled manner to direct endogenous cell function. To prove the role of this adaptive release system, we applied the polyelectrolyte coating on a well-studied biodegradable poly(lactic-co-glycolic acid) support membrane. The released growth factors directed cellular processes to induce bone repair in a critical-size rat calvaria model. The released growth factors promoted local bone formation that bridged a critical-size defect in the calvaria as early as 2 wk after implantation. Mature, mechanically competent bone regenerated the native calvaria form. Such an approach could be clinically useful and has significant benefits as a synthetic, off-the-shelf, cell-free option for bone tissue repair and restoration.