Growing functional vocal cords in the lab
November 19, 2015
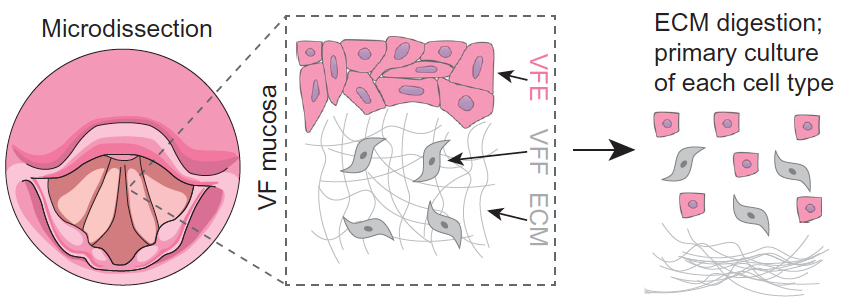
Extracting fibroblasts and epithelial cells from donor vocal fold mucosa for culturing and application to a 3-D collagen scaffold (credit: Changying Ling et al./Tissue Engineering)
University of Wisconsin scientists have succeeded in growing functional vocal-cord tissue in the laboratory and bioengineering it to transmit sound, a major step toward restoring voice for people who have lost their vocal cords to cancer surgery or other injuries.
Dr. Nathan Welham, a speech-language pathologist and an associate professor of surgery in the UW School of Medicine and Public Health, and colleagues began with vocal-cord tissue from a cadaver and four patients who had their larynxes removed but did not have cancer. They isolated, purified, and grew the cells from the mucosa, then applied them to a 3-D collagen scaffold, similar to a system used to grow artificial skin in the laboratory.
In about two weeks, the cells grew together to form a tissue with a pliable but strong connective tissue beneath, and layered epithelial cells on top. Proteomic analysis showed the cells produced many of the same proteins as normal vocal cord cells. Physical testing showed that the epithelial cells had also begun to form an immature basement membrane which helps create a barrier against pathogens and irritants in the airway.
“Normal sound output”
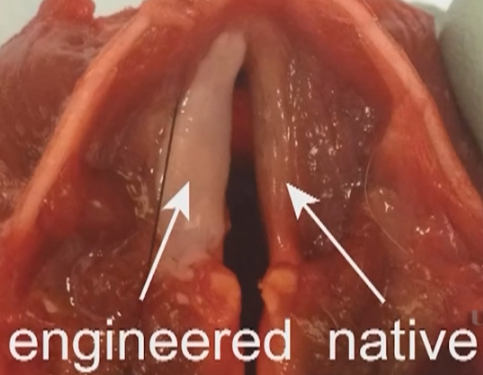
Engineered vocal-cord tissue in lab (credit: UW School of Medicine and Public Health)
After testing in cadaver dogs, the researchers tested the tissue for rejection or acceptance using mice that had been engineered to have human immune systems. The tissue grew and was not rejected.
In one way, the tissue was not as good as the real thing: its fiber structure was less complex than adult vocal cords, but the authors said this was not surprising because human vocal cords continue to develop for at least 13 years after birth. But Welham said the tissue had “normal sound output” in lab tests.
Welham says vocal-cord tissue that is free of cancer is a rare commodity, so clinical applications will either require banking and expansion of human cells, or the use of stem cells derived from bone marrow or other tissues. Stem cells could be primed to differentiate into vocal-cord cells by exposing them to vibration and tensile forces in a “laryngeal bioreactor.”
Clinical applications are still years away, but Welham says this proof-of-principle study is a “robust benchmark” along the route to replacement vocal-cord tissue. Moving this promising work forward requires more testing of safety and long-term function. “Our vocal cords are made up of special tissue that has to be flexible enough to vibrate, yet strong enough to bang together hundreds of times per second. It’s an exquisite system and a hard thing to replicate.”
About 20 million Americans suffer from voice impairments, and many have damage to the vocal-cord mucosae, the specialized tissues that vibrate as air moves over them, giving rise to voice. While injections of collagen and other materials can help some in the short term, not much can be done currently for people who have had larger areas of their vocal cords damaged or removed, Welham says.
The study was published in the journal Science Translational Medicine.
UWMedicine | Engineered Vocal Fold Tissue
Abstract of Bioengineered vocal fold mucosa for voice restoration
The power of the voice cannot be disputed. For instance, Adele’s lyrics would not elicit chills (or tears) without strategic pitch and harmonizing known as appoggiatura; the chant “Yes we can” garnered more than 69 million popular votes to win Obama the 2008 presidential election; and, more simply, voice is the primary means we all use to communicate with co-workers, loved ones, and the rest of society. Dysphonia—or difficulty speaking from vocal fold tissue damage or loss—can impair one’s ability to be an effective communicator. To provide a new option for those with dysphonia, Ling et al. used two different types of human vocal fold cells to create a functional mucosa. When grafted into the dog larynx ex vivo, the engineered vocal fold reproduced natural physiology, including the vibrations necessary to transmit sound. In vivo, in humanized mice, the engineered mucosa was tolerated by functional human immune cells. These data suggest feasibility for transplant and survival in the larynx as well as for function, ultimately giving patients back their voices.