How to quickly generate a large quantity of personalized nerve cells
June 14, 2013
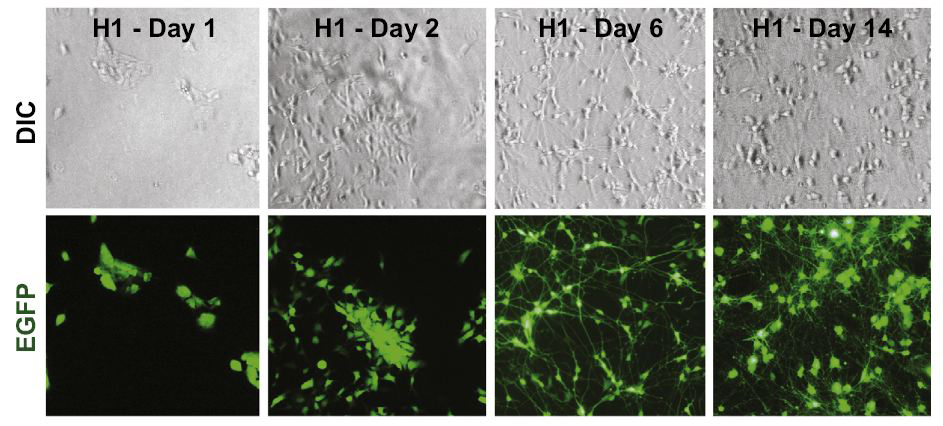
Representative images illustrating the time course of the conversion of H1 ESCs (stem cells) into iN (nerve) cells. Corresponding differential interference contrast (DIC) and GFP fluorescence pictures are shown on top and bottom. (Credit: Yingsha Zhang et al./Neuron)
A team under the direction of Stanford cell physiologist and neuroscientist Tom Sudhof, PhD, has shown that in human ESCs or iPSCs, just boosting the level of a single transcription factor results in an abundant and quite pure population of nerve cells within as little as two weeks.
And unlike previous methods, this one seems to generate nerve cells of equally high functional quality regardless of which “starter” cell line was used to get the process underway.
Clearly, if you’re doing regenerative medicine for a stroke or brain-trauma victim etc., you’re going to need a lot of nerve cells, and time is of the essence. So the new method represents a major forward step toward the realization of the dream of personalized regenerative medicine.
Why ESCs and iPSCs are important
Embryonic stem cells (or ESCs) and their younger cousins the induced pluripotent stem cells (iPSCs) are prized because they can, alternatively, replicate themselves indefinitely in a dish or differentiate into every cell type in the body. This makes them potentially valuable tools for regenerative medicine.
And because iPSCs can be made from a person’s skin cells, manipulating their differentiated progeny lets investigators study disease processes at the cellular level, in a dish and in a personalized way. By custom-producing, for example, a given individual’s nerve cells, researchers can study the specific defects of those cells in a dish, without having to first perform the ethically unthinkable — and, therefore, purely hypothetical — act of slicing chunks of tissue out of that person’s brain in order to do so.
The researchers can, further, toss thousands of different compounds into thousands of tiny “wells” containing these nerve cells to see which ones might restore those cells’ proper function. (Different drugs are likely to work better with different individuals’ defective cells, depending on the nature of the cell’s defining defect.)
Previous problems
Scientists have successfully coaxed both ESCs and iPSCs down the developmental pathway to become nerve cells. They’ve even generated nerve cells directly from skin cells. But up to now, the procedures they’ve used have been plagued by two problems.
- Quality assurance: the extent to which nerve cells generated by these methods actually look and act like nerve cells are supposed to look and act varies a lot, depending on which particular ESC line, or which iPSC line, was used to generate them.
- The process is slow and the yield is low (it typically takes months to get from the beginning to the end, and many of the “starter” ESCs or iPSCs don’t successfully convert to decently functioning nerve cells).