New evidence that electrical stimulation accelerates wound healing
May 15, 2015
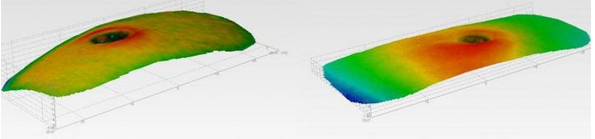
An untreated wound (left) after 10 days is larger than an electrical-stimulation-treated wound (right) (credit: The University of Manchester)
The most detailed study to date of skin wound healing, conducted by University of Manchester scientists with 40 volunteers, has provided new evidence that electrical stimulation accelerates wound healing.
In the new research, half-centimeter harmless wounds were created on each upper arm of the volunteers. One wound was left to heal normally, while the other was treated with electrical pulses* over a period of two weeks. The pulses stimulated angiogenesis — the process by which new blood vessels form — increasing blood flow to the damaged area and resulting in wounds healing significantly faster.

Normal-healing tissues (top) vs. electrical-stimulation-treated healing tissues (bottom). Electrical-stimulation sample showed reorganization and accelerated granulation tissue stage development. ED is epidermis, DE is dermis, GT is granulation tissue, FT is fat/adipose tissue. (credit: Sara Ud-Din et al./PLoS ONE)
“The aim of this study was to further evaluate the role of electrical stimulation (ES) in affecting angiogenesis during the acute phase of cutaneous wound healing over multiple time points to identify if the enhanced effect occurred earlier than day 14,” the researchers note in a paper published in open-access PLoS ONE.
“This research has shown the effectiveness of electrical stimulation in wound healing,” said research leader Ardeshir Bayat of the University’s Institute of Inflammation and Repair. “We believe this technology has the potential to be applied to any situation where faster wound healing is particularly desirable, such as human or veterinary surgical wounds, accidents, military trauma, and sports injuries.”
Based on the findings, the researchers plan to work with Oxford BioElectronics Ltd. on a five-year project to develop and evaluate devices and dressings that use these experimental techniques to stimulate the body’s nervous system to generate nerve impulses directed to the site of skin repair.
How electrical stimulation enhances wound healing
The researchers explain in the paper that “ES in its various forms has been shown to enhance wound healing by promoting the migration of keratinocytes and macrophages, enhancing angiogenesis, stimulating fibroblasts, and influencing protein synthesis throughout the inflammatory, proliferative, and remodeling phases of healing.”
The researchers previously “investigated the in vitro effect of different types of ES on the expression of collagen in skin fibroblasts. Importantly, we highlighted the role of a novel waveform termed degenerate wave (DW is a degenerating sine wave, which deteriorates over time) and demonstrated its beneficial effects compared to other known waveforms such as direct and alternating currents.”
Skin wounds that are slow to heal are a clinical challenge to physicians all over the world. Every year, the NHS in the U.K. alone spends £1 billion on treating chronic wounds such as lower limb venous and diabetic ulcers. (Wounds become chronic when they fail to heal and remain open for longer than six weeks.)
* According to the researchers writing in the PLoS ONE paper, the electrical stimulation device used was the Fenzian system (Fenzian Ltd, Hungerford, UK), a transcutaneous low intensity device that detects changes in skin impedance and adjusts the outgoing microcurrent electrical biofeedback impulses (20–80V, 6-millisecond “degenerate wave” pulses at 0.004 milliamps, with a frequency default of 60Hz).
Abstract of Angiogenesis Is Induced and Wound Size Is Reduced by Electrical Stimulation in an Acute Wound Healing Model in Human Skin
Angiogenesis is critical for wound healing. Insufficient angiogenesis can result in impaired wound healing and chronic wound formation. Electrical stimulation (ES) has been shown to enhance angiogenesis. We previously showed that ES enhanced angiogenesis in acute wounds at one time point (day 14). The aim of this study was to further evaluate the role of ES in affecting angiogenesis during the acute phase of cutaneous wound healing over multiple time points. We compared the angiogenic response to wounding in 40 healthy volunteers (divided into two groups and randomised), treated with ES (post-ES) and compared them to secondary intention wound healing (control). Biopsy time points monitored were days 0, 3, 7, 10, 14. Objective non-invasive measures and H&E analysis were performed in addition to immunohistochemistry (IHC) and Western blotting (WB). Wound volume was significantly reduced on D7, 10 and 14 post-ES (p = 0.003, p = 0.002, p<0.001 respectively), surface area was reduced on days 10 (p = 0.001) and 14 (p<0.001) and wound diameter reduced on days 10 (p = 0.009) and 14 (p = 0.002). Blood flow increased significantly post-ES on D10 (p = 0.002) and 14 (p = 0.001). Angiogenic markers were up-regulated following ES application; protein analysis by IHC showed an increase (p<0.05) in VEGF-A expression by ES treatment on days 7, 10 and 14 (39%, 27% and 35% respectively) and PLGF expression on days 3 and 7 (40% on both days), compared to normal healing. Similarly, WB demonstrated an increase (p<0.05) in PLGF on days 7 and 14 (51% and 35% respectively). WB studies showed a significant increase of 30% (p>0.05) on day 14 in VEGF-A expression post-ES compared to controls. Furthermore, organisation of granulation tissue was improved on day 14 post-ES. This randomised controlled trial has shown that ES enhanced wound healing by reduced wound dimensions and increased VEGF-A and PLGF expression in acute cutaneous wounds, which further substantiates the role of ES in up-regulating angiogenesis as observed over multiple time points. This therapeutic approach may have potential application for clinical management of delayed and chronic wounds.