Replacing a defective gene with a correct sequence to treat genetic disorders
April 10, 2014
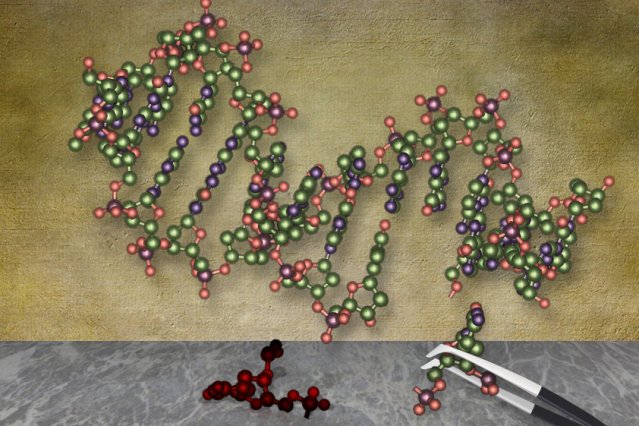
(Credit: Christine Daniloff/MIT)
Using a new gene-editing system based on bacterial proteins, MIT researchers have cured mice of a rare liver disorder caused by a single genetic mutation.
The findings, described in the March 30 issue of Nature Biotechnology, offer the first evidence that this gene-editing technique, known as CRISPR, can reverse disease symptoms in living animals. CRISPR, which offers an easy way to snip out mutated DNA and replace it with the correct sequence, holds potential for treating many genetic disorders, according to the research team.
“What’s exciting about this approach is that we can actually correct a defective gene in a living adult animal,” says Daniel Anderson, the Samuel A. Goldblith Associate Professor of Chemical Engineering at MIT, a member of the Koch Institute for Integrative Cancer Research, and the senior author of the paper.
The recently developed CRISPR system relies on cellular machinery that bacteria normally use to defend themselves from viral infection. Researchers have copied this cellular system to create new gene-editing complexes, which include a DNA-cutting enzyme called Cas9 bound to a short RNA guide strand. The strand is programmed to bind to a specific genome sequence, telling Cas9 where to make its cut.
At the same time, the researchers also deliver a DNA template strand. When the cell repairs the damage produced by Cas9, it copies from the template, introducing new genetic material into the genome. Scientists envision that this kind of genome editing could one day help treat diseases such as hemophilia, Huntington’s disease, and others that are caused by single mutations.
“The CRISPR system is very easy to configure and customize,” says Anderson, who is also a member of MIT’s Institute for Medical Engineering and Science. He adds that other systems “can potentially be used in a similar way to the CRISPR system, but with those it is much harder to make a nuclease that’s specific to your target of interest.”
Disease correction
For this study, the researchers designed three guide RNA strands that target different DNA sequences near the mutation that causes type I tyrosinemia, in a gene that codes for an enzyme called FAH. Patients with this disease, which affects about 1 in 100,000 people, cannot break down the amino acid tyrosine, which accumulates and can lead to liver failure. Current treatments include a low-protein diet and a drug called NTCB, which disrupts tyrosine production.
To deliver the CRISPR components, the researchers employed a technique known as high-pressure injection, which uses a high-powered syringe to rapidly discharge the material into a vein. This approach delivers material successfully to liver cells, but Anderson envisions that better delivery approaches are possible. His lab is now working on methods that may be safer and more efficient, including targeted nanoparticles.
Researchers at Koch Institute, the Oregon Stem Cell Center, and Skolkovo Institute of Science and Technology were also involved in the study. The research was funded by the National Cancer Institute, the National Institutes of Health, and the Marie D. and Pierre Casimir-Lambert Fund.
Abstract of Nature Biotechnology paper
We demonstrate CRISPR-Cas9–mediated correction of a Fah mutation in hepatocytes in a mouse model of the human disease hereditary tyrosinemia. Delivery of components of the CRISPR-Cas9 system by hydrodynamic injection resulted in initial expression of the wild-type Fah protein in ~1/250 liver cells. Expansion of Fah-positive hepatocytes rescued the body weight loss phenotype. Our study indicates that CRISPR-Cas9–mediated genome editing is possible in adult animals and has potential for correction of human genetic diseases.