Respirocytes
May 20, 2002 by Robert A. Freitas Jr.
An artificial nanomedical erythrocyte, or “respirocyte” — intended to duplicate all of the important functions of the red blood cell — could serve as a universal blood substitute, preserve living tissue, eliminate “the bends,” allow for new sports records, and provide treatment for anemia, choking, lung diseases, asphyxia, and other respiratory problems.
Based on an article by Robert A. Freitas Jr. written in 2001. Published on KurzweilAI.net May 20, 2002.
Molecular manufacturing promises precise control of matter at the atomic and molecular level. Sometime in the next 10-30 years it may become possible to construct machines on the microscopic (1 micron = 10-6 meter) scale, comprised of parts on the nanometer (10-9 meter) scale. Such tiny machines may be built by assembling in a single device such useful components as 100-nanometer robotic manipulator arms, mechanical GHz-clock computers occupying a cube only 400 nanometers on an edge, sorting rotors for molecule-by-molecule reagent purification spanning a mere 10 nanometers in diameter, and smooth superhard surfaces made of atomically flawless diamond.
These bacterium-sized nanorobots will profoundly impact the practice of medicine – nanomedicine – in the early 21st century. For the first time, physicians will be able to perform precise interventions at the cellular and molecular level. The most advanced nanomedical devices may be used to diagnose and cure bacterial and viral infections, destroy cancerous tumors, eliminate heart disease, undo metabolic deficiencies, repair physically injured limbs and organs, reverse some forms of neural damage, arrest the aging process, and even restore normal cellular functions after a lengthy cryogenic suspension.
However, nanotechnology is such a powerful tool that a little bit goes a long way. Even seemingly modest machines may have many applications beyond those that are immediately apparent. To demonstrate this, in 1995-1996 I did a detailed design analysis of a relatively simple nanomedical device – an artificial mechanical erythrocyte, or “respirocyte” – intended to duplicate all of the important functions of the most common cell in the human body, the red blood cell.
WHAT RED CELLS DO
Red cells comprise at least 80% of all native cells in the human body. These cells have many useful functions, but they have two most important tasks. First, they must transport respiratory gases throughout the body. Second, they must help prevent the blood from becoming too acidic, since carbon dioxide dissolved in water is an acid.
The biochemistry of respiratory gas transport in the blood is well understood. In brief, oxygen and carbon dioxide (the chief byproduct of the combustion of foodstuffs) are carried between the lungs and the other tissues, mostly within the red blood cells. Hemoglobin, the principal protein in the red blood cell, combines reversibly with oxygen, forming oxyhemoglobin. About 95% of the O2 is carried in this form, the rest being dissolved in the blood. At human body temperature, the hemoglobin in 1 liter of blood holds 200 cm3 of oxygen, 87 times more than plasma alone (2.3 cm3) can carry.
Carbon dioxide also combines reversibly with hemoglobin, forming carbamino hemoglobin. About 25% of the CO2 produced during cellular metabolism is carried in this form, with another 65% transported inside the red cells as bicarbonate ion and the remaining 10% dissolved in blood plasma. The creation of carbamino hemoglobin and bicarbonate ion releases hydrogen ions, which, without hemoglobin, would leave venous blood 800 times more acidic than the arterial. This does not happen because hemoglobin reversibly absorbs the excess hydrogen ions, mostly within the red blood cells.
Respiratory gases are taken up or released by hemoglobin according to their local partial pressure. There is a reciprocal relation between hemoglobin’s affinity for oxygen and carbon dioxide. The relatively high level of O2 in the lungs aids the release of CO2, which is to be expired. The high CO2 level in other tissues aids the release of O2 for use by those tissues.
DESIGNING AN ARTIFICIAL RED CELL
Once we have the ability to precisely engineer complex, micron-scale machines, what is the best way to go about designing an artificial red blood cell? Given our goal of oxygen transport from the lungs to other body tissues, the simplest possible design is a microscopic pressure vessel, spherical in shape for maximum compactness.
Most proposals for durable nanostructures employ the strongest materials, such as flawless diamond or sapphire, constructed atom by atom. A conservative working stress in such structures would be about 100,000 atmospheres (atm) of pressure. But rupture risk and explosive energy rise with pressure, so a standard 1000 atm peak operating pressure appears optimum. This relatively low pressure still offers a very high packing density of the gas molecules, while providing an extremely conservative 100-fold structural safety margin. By comparison, natural red blood cells store oxygen at an equivalent 0.51 atm pressure, of which only 0.13 atm is deliverable to tissues.
How would these microscopic pressure tanks work? In the simplest case, oxygen release could be continuous throughout the body. Slightly more sophisticated would be a system that releases gas in response to local O2 partial pressure. But these simple proposals fall short on two counts.
First, once discharged the devices become useless. And the discharge time is way too short. If there were no natural red cells around to help out, the O2 contained in a 1 cm3 injection of 1000 atm microtanks would be exhausted in only 2 minutes.
Second, placement of lots of point sources of oxygen emission throughout the capillary bed, side by side with the existing red cell population, would cause a serious problem. These extra emitters are functionally equivalent to red blood cells whose CO2 transport and acid-buffering capabilities have been selectively disabled. Their addition to the blood pushes respiratory gas equilibrium toward higher CO2 tension and elevated hydrogen ion concentration. These higher concentrations would rapidly lead to carbon dioxide toxicity and acidosis (hypercapnia), especially in anemic, nonrespiratory, or ischemic patients, as well as hyperoxic hemolysis and other complications.
The solution to the problem of short duration is to continuously recharge the microvessels with oxygen gas at the lungs. We can also prevent carbon dioxide toxicity by providing extra tankage for CO2 transport and by designing a mechanism that actively loads the gas in the tissues and then unloads it at the lungs.
The key to successful respirocyte function is to provide some active means of conveying gas molecules into, and out of, pressurized microvessels. K. Eric Drexler (Nanosystems, 1992) has proposed molecular sorting rotors that would be ideal for this task. Each rotor has binding site “pockets” along the rim exposed alternately to the blood plasma and the interior chamber by the rotation of the disk. While exposed to blood plasma, a pocket selectively binds a specific molecule like oxygen or carbon dioxide. The disk then rotates so that the loaded binding site moves into the interior chamber. Once the pocket has moved into the chamber, the bound molecule is forcibly ejected by a rod thrust outward by the cam surface. Enzymatic binding sites for oxygen, carbon dioxide, nitrogen, water and glucose are already well known.
Molecular sorting rotors can be designed from about 100,000 atoms (including the housing), measuring roughly 7 nm x 14 nm x 14 nm in size with a mass of 2 x 10-21 kg. These minute devices could pump small molecules of 20 or fewer atoms at a rate of 1 million molecules/sec against head pressures up to 30,000 atm. Rotors are fully reversible, so they can be used to load or unload gas storage tanks, depending upon the direction of rotor rotation.
How big should our artificial red cell be? The upper limit is easy to specify because respirocytes must have ready access to all tissues via blood vessels. They cannot be larger than human capillaries which average 8 microns in diameter but may be as small as 4 microns – so narrow that natural red blood cells (7.8 micron x 2.6 micron biconcave disks) must fold in half to pass, single-file.
As design radius shrinks, surface area per unit enclosed volume rises rapidly. Thus smaller cells require more hollow tankage structural mass for a given amount of volume capacity. A careful study of operational requirements and minimum component sizes suggests that the optimum respirocyte diameter is about 1 micron.
Another design issue is buoyancy, which is easily controlled by loading or unloading water ballast. Why is this important? Active ballast management is crucial when it comes time to remove respirocytes from a patient’s blood. In one method, called “nanapheresis,” devices are removed by passing the blood from a catheterized patient into a specialized centrifugation apparatus where acoustic transmitters command respirocytes to establish neutral buoyancy. No other solid blood component can maintain exact neutral buoyancy as a respirocyte can. As a result, all non-respirocyte blood components precipitate outward during gentle centrifugation and are drawn off and added back to filtered plasma on the other side of the apparatus. Meanwhile, after a period of centrifugation, the plasma, containing mostly suspended respirocytes but few other solids, is drawn off through a 1-micron filter, removing the respirocytes. The reconstituted whole blood returns undamaged to the patient’s body. (Other more elegant removal methods exist, but nanapheresis is easiest to explain and would clearly work.)
RESPIROCYTES
The artificial respirocyte is a hollow, spherical nanomedical device 1 micron in diameter. The respirocyte is built of 18 billion precisely arranged structural atoms, and holds an additional 9 billion molecules when it is fully loaded. Each main storage tank – one for oxygen (up to ~1.5 billion molecules), another for carbon dioxide (up to ~1.5 billion molecules), and a third for ballast water (up to ~6 billion molecules) – is constructed of diamondoid honeycomb or a geodesic grid skeletal framework for maximum strength. Thick diamond bulkheads separate internal tankage volumes, and a universal “bar code” is embossed on either side of the device.
An onboard chemomechanical turbine or fuel cell generates power by combining glucose drawn from the bloodstream and oxygen drawn from internal storage. This is converted to mechanical power which drives molecular sorting rotors and other subsystems, as demonstrated in principle by a variety of biological motor systems such as bacteria flagella. Each powerplant develops 0.3 picowatts of power. That’s enough energy to fill the oxygen tank in 10 seconds from empty, a pumping rate of 100 million molecules/sec. One powerplant measures 42 nm x 42 nm x 175 nm in size, constructed of 100 million atoms weighing ~10-18 kg. Power is transmitted mechanically or hydraulically using an appropriate working fluid. Power is distributed with sliding rods and gear trains, or using pipes and mechanically operated valves, and is controlled by the computer.
The attending physician broadcasts his/her commands to molecular mechanical systems deployed in the human body by sending messages impressed on modulated compressive pressure pulses, which are received by mechanical acoustic transducers embedded in the surface of the respirocyte. Converting a pattern of pressure fluctuations into mechanical motions that can serve as input to a mechanical computer requires transducers that function as pressure-driven actuators. These actuators measure 20-30 nanometers in size.
We also need various sensors to acquire external data needed to regulate gas loading and unloading operations, tank volume management, and other special protocols. For instance, we can design quantitative concentration sensors for any molecular species desired using a special type of sorting rotor that includes a probe that can determine whether or not a binding pocket is filled, thus giving the rotor the ability to count. It is also convenient to include internal pressure sensors to monitor O2 and CO2 gas tank loading, ullage sensors for ballast and glucose fuel tanks, and internal/external temperature sensors to help monitor and regulate total system energy output.
An onboard computer is necessary for precise control of respiratory gas loading and unloading, rotor field and ballast tank management, powerplant throttling, power distribution, interpretation of sensor data and commands received from the outside, self-diagnosis and activation of failsafe shutdown protocols, and ongoing revision or correction of protocols in vivo. A 10,000 bit/sec computer can probably meet all computational requirements, given the simplicity of analogous chemical process control systems in factory settings. That’s roughly the computing capacity of a transistor-based 1960-vintage IBM 1620 computer, or about 1/50th the capacity of a 1976-vintage Apple II microprocessor-based PC.
Twelve pumping stations are spaced evenly along an equatorial circle. Each station has its own independent glucose powerplant, glucose tank, environmental glucose sensors, and glucose sorting rotors. Any one station acting alone can generate sufficient energy to power the entire respirocyte. Power is transmitted hydraulically or by cables to local station subsystems and also along a dozen independent interstation trunk lines that allow stations to pass mechanical power among themselves as required, permitting load shifting and balancing.
Each pumping station has an array of 3-stage molecular sorting rotor assemblies for pumping oxygen, carbon dioxide, and water into and out of the ambient medium. The number of rotors in each array is determined both by performance requirements and by the anticipated concentration of each target molecule in the bloodstream. Any one pumping station, acting alone, can load or discharge any storage tank in ~10 sec (typical capillary transit time in tissues), whether gas, ballast water, or glucose. Gas pumping rotors are arrayed in a noncompact geometry to minimize the possibility of local molecule exhaustion during loading.
The system presented here has at least tenfold redundancy in all components. This should suffice to reduce system failure to negligible levels. For example, ten duplicate computer/mass-memory sets are located at the center of the device in a spherical 1 million nm3 volume. Any of the 10 computers at the core can receive power or communications directly from any of the 12 pumping stations along hard links in protected utility conduits.
HOW DO THEY WORK?
The average male human body has 28.5 trillion red blood cells, each containing 270 million hemoglobin molecules binding four O2 molecules per hemoglobin. However, since hemoglobin normally operates between 95% saturation (arterial) and 70% saturation (venous), only 25% of stored oxygen is accessible to the tissues.
By contrast, each respirocyte stores up to 1.51 billion oxygen molecules, 100% of which are accessible to the tissues. To fully duplicate human blood active capacity, we have to deploy 5.36 trillion devices. If respirocytes are administered via hypodermal injection or transfusion in a 50% aqueous colloidal suspension, this requires a standard ~5.61 cm3 therapeutic dose of activated suspension, taking only seconds to inject at, say, an accident scene. One therapeutic dose can duplicate natural red cell function indefinitely if the patient is breathing. It can supply all respiratory gas requirements from onboard storage alone for nearly 2 minutes for patients who are not breathing.
But one of the potential benefits of nanomedical devices is their ability to extend natural human capabilities. Suppose you wanted to permanently maximize the oxygen-carrying capacity of your blood by infusing the largest possible number of respirocytes. The maximum safe augmentation dosage is probably about 1 liter of 50% respirocyte suspension, which puts 954 trillion devices into your bloodstream. You could then hold your breath for 3.8 hours, at the normal resting metabolic rate. At the maximum human metabolic rate, something like a continuous Olympic-class 50-meter dash exertion level, you could go for a full 12 minutes without taking a breath. Afterwards, your entire capacity is recharged by hyperventilating for just 8 minutes – then you’re ready to go again.
ARE THEY SAFE?
Respirocyte self-diagnostic routines will detect simple failure modes like jammed rotor banks, plugged exhaust ports, and gas leaks, either switching to backup systems or using those backups to safely place the device into a fail-safe dormant mode pending removal by filtration. Respirocytes should be extremely reliable. A simple analysis of likely radiation damage suggests that the average respirocyte should last about 20 years before failing.
What if all 12 glucose powerplants jam on and refuse to turn off? If this malfunction occurs while the respirocyte is in your bloodstream, its temperature won’t rise at all. That’s because the 7.3 picowatts of continuous thermal energy the device is generating is easily absorbed by the huge aqueous heat sink, which has a bountiful heat capacity.
Can respirocytes explode? Each device contains up to 0.24 micron3 of oxygen and carbon dioxide gas at 1000 atm pressure, representing 24 picojoules of stored mechanical energy. If the device explodes in air the shrapnel travels outward at ~257 m/sec, slower than the speed of sound in air (331 m/sec) so there is no acoustic shock wave – it will hiss, not snap. If the device explodes inside human tissue, the gases do work against the surrounding fluid, displacing 10-16 meter3 of water while raising the water’s temperature only 0.04°C and expanding to a bubble 6 microns in diameter, just 2% the volume of a typical human cell. Since the average separation of neighboring respirocytes in the blood is 2-10 microns (depending on dosage), such gas bubbles should be reabsorbed almost immediately. So single-device explosions are unlikely to cause embolic or other significant damage.
Short of manufacturing defect, it’s pretty hard to imagine a scenario that leads to complete structural failure of a respirocyte in vivo. Patients suffering a multistory fall onto a concrete pavement or a high-speed head-on automobile collision experience instantaneous accelerations of 100-10,000 g’s (gravity is 1 g), but a spherical diamondoid shell should resist accelerations up to 108-1010 g’s. Crushing respirocyte-impregnated human tissue in a hydraulic press is unlikely to destroy any devices, as they will simply slide out of the way. The same logic applies to gunshot wounds, knife accidents that cut deep to hard bone, and blunt object blows to the skull.
Indeed, the only plausible respirocyte explosion scenario is dental grinding. That’s because tooth enamel is the hardest natural substance in the human body, and a patient with an oral lesion could spread respirocyte-impregnated blood over the teeth. Single-device explosions may not be detectable; several thousand going off at once might produce a “fizziness” in the mouth. Simultaneously crushing 20 million respirocytes (the count in a 0.5-mm droplet of augmentation-dose blood) could produce a maximum jaw-speed (0.1 m/sec) explosive impulse. But this requires the out-of-bloodstream protocol to have failed simultaneously in all devices, an extremely unlikely event.
Collisions with respirocytes or their spinning sorting rotors are unlikely to cause serious physical damage to other cells in the bloodstream such as platelets, white cells, or natural red cells, nor will collisions injure blood vessel walls. While definitive experimental data is not yet available, preliminary tests show diamondoid surfaces to be very biocompatible, unlikely to draw a major response from leukocytes, the immune system, or other natural body defenses.
LOTS OF APPLICATIONS
The mechanical respirocyte may be used as the active oxygen-carrying component of a universally transfusable blood substitute certifiably free of disease vectors such as hepatitis, venereal diseases, malarial parasites or AIDS. It is storable indefinitely and readily available to recipients of all blood types. Organ donation will also get a boost. In current practice, organs must be transplanted soon after harvest. Respirocytes could be employed as a long-duration perfusant to preserve living tissue, especially at low temperature, for grafts (kidney, marrow, liver and skin) and for organ transplantation.
Respirocytes could also be used as a complete or partial symptomatic treatment for virtually all forms of anemia. The devices are a good preventative treatment for perinatal and neonatal disorders such as Sudden Infant Death Syndrome (SIDS) or crib death, the leading cause of neonatal death (~5000/yr in the U.S.) between 1 week and 1 year of age. Respirocytes would help treat a wide variety of lung diseases and conditions ranging in severity from hay fever, asthma and snoring to tetanus, pneumonia and polio. The devices could also contribute to the success of certain extremely aggressive cardiovascular and neurovascular procedures, tumor therapies and diagnostics.
Respirocytes make it possible to breathe in oxygen-poor environments, or in situations where normal breathing is physically impossible. Prompt injection with a therapeutic dose, or advance infusion with an augmentation dose, could greatly reduce the number of choking deaths (~3200 deaths/yr in U.S.) and reduce the use of emergency tracheostomies, artificial respiration in first aid, and mechanical ventilators. The device would provide an excellent prophylactic treatment for most forms of asphyxia, especially those involving drowning, strangling, electric shock (respirocytes are purely mechanical), nerve-blocking paralytic agents, carbon monoxide poisoning, underwater rescue operations, smoke inhalation or firefighting activities, anesthetic/barbiturate overdose, confinement in airtight spaces (refrigerators, closets, bank vaults, mines, submarines), or obstruction of breathing (by a chunk of meat or a plug of chewing tobacco lodged in the larynx, by inhalation of vomitus, or by a plastic bag pulled over the head of a child).
Then there is the “nanolung.” An interesting design alternative to augmentation infusions is a therapeutic population of respirocytes that loads and unloads at an artificial nanolung, a diamondoid pressure tank implanted in the chest, which exchanges gases directly with the natural lungs or with an external gas supply such as an air hose. Assuming 80% storage volume at ~1000 atm, an unobtrusive 250 cm3 nanolung could provide 0.3-7 hours O2 supply, depending on exertion level. By sacrificing one entire natural lung to make room in the thorax, a 3250 cm3 nanolung extends oxygen supply to 4-87 hours. A less-conservative nanolung design could allow you to survive for up to 5 days without drawing a breath.
Respirocytes could serve as in vivo SCUBA (Self-Contained Underwater Breathing Apparatus) devices. Using an augmentation dose of respirocytes or a nanolung, the diver simply holds his breath and dives, goes about his business underwater for a few hours, then surfaces, hyperventilates for 8 minutes to recharge, and returns to work below. (Similar considerations would apply while living and working in space.) Unfortunately, direct water-breathing for extended periods of time, even with the help of respirocytes, does not appear technically feasible.
Respirocytes can also relieve the most dangerous hazard of deep sea diving – decompression sickness (“the bends”) or caisson disease, caused by the formation of nitrogen bubbles in blood as a diver rises to the surface. These bubbles come from gas previously dissolved in the blood at higher pressure at greater depths. Safe decompression procedures normally require up to several hours. But a small therapeutic dose of respirocytes reconfigured to absorb nitrogen instead of O2/CO2 gases could allow safe and complete decompression of an N2-saturated human body from a depth of 26 meters (86 feet) in as little as 1 second. (In practice, full relief may require ~60 sec approximating the circulation time of the blood.) Each additional therapeutic dose relieves excess N2 accumulated from another 16 meters of depth.
Respirocytes could permit the achievement of major new sports records. That’s because the devices can deliver oxygen to muscle tissue faster than the lungs can provide, for the duration of the sporting event. Indeed, our baseline respirocyte can deliver 236 times more oxygen to the tissues per unit volume than natural red cells, and enjoys a similar advantage in carbon dioxide transport. This would be especially useful in running, swimming, and other endurance-oriented events, and in competitive sports such as basketball, football and soccer where extended periods of sustained maximum exertion are required.
Artificial blood substitutes may also have wide use in veterinary medicine, especially in cases of vehicular trauma and kidney failure where transfusions are required, and in battlefield applications demanding blood replacement or personnel performance enhancement. Swallowed in pill form, respirocytes could be an effective, though temporary, cure for flatulence, which is largely swallowed air and CO2 generated by fermentation in the stomach. With suitable modifications, future respirocyte technology could provide a precisely timed or scheduled ingestible or injectable drug delivery system. The devices could also help manage serum glycerides, fatty acids or lipoproteins, metabolic disorders like diabetic ketosis and gestational diabetes, and other undesired dietary conditions.
NOTE: For a more detailed analysis of the proposed respirocyte device and a comprehensive discussion of many technical and medical issues not touched upon here (including 173 references and 14 tables/figures), the interested reader may consult “A Mechanical Artificial Red Cell: Exploratory Design in Medical Nanotechnology” at http://www.foresight.org/Nanomedicine/Respirocytes.html. This is the original version of the refereed paper describing respirocytes that was submitted for publication on 17 April 1996. A shorter version of this paper – the first nanorobot technical design study ever published in a peer-reviewed medical journal – was published in 1998 as: Robert A. Freitas Jr., “Exploratory Design in Medical Nanotechnology: A Mechanical Artificial Red Cell,” Artificial Cells, Blood Substitutes, and Immobil. Biotech. 26(1998): 411-430. Images of the respirocyte design may be found online at my Nanomedicine Art Gallery, located at http://www.foresight.org/Nanomedicine/Gallery/index.html.
© 2001 Robert A. Freitas Jr. All Rights Reserved. Reprinted with permission.
Footnotes
Respirocyte animation wins IMM Computational Nanotechnology Prize
Oct. 17, 2002 — Phlesch Bubble has been awarded the Institute for Molecular Manufacturing (IMM) Computational Nanotechnology Prize (Simulation category) for their animation of a respirocyte (a hypothetical artificial red blood cell), designed by Robert A. Freitas Jr.
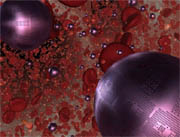 A respirocyte releasing oxygen in an arteriole. Click here to view the QuickTime animation.
A respirocyte releasing oxygen in an arteriole. Click here to view the QuickTime animation.
"The animation starts with a suspension of respirocytes being injected into a smoke-inhalation victim," Phlesch Bubble’s Jillian Rose explained to KurzweilAI.net.
"We follow the respirocytes as they progress from artery to arteriole to capillary. In the capillary we focus on the mechanics of the respirocyte at the molecular scale, as its sorting rotors release oxygen into and capture carbon dioxide from the bloodstream."