round-up | Two new wearable sensors may replace traditional medical diagnostic devices
February 21, 2018
Throat-motion sensor monitors stroke effects more effectively
A radical new type of stretchable, wearable sensor that measures vocal-cord movements could be a “game changer” for stroke rehabilitation, according to Northwestern University scientists. The sensors can also measure swallowing ability (which may be affected by stroke), heart function, muscle activity, and sleep quality. Developed in the lab of engineering professor John A. Rogers, Ph.D., in partnership with Shirley Ryan AbilityLab in Chicago, the new sensors have been deployed to tens of patients.
“One of the biggest problems we face with stroke patients is that their gains tend to drop off when they leave the hospital,” said Arun Jayaraman, Ph.D., research scientist at the Shirley Ryan AbilityLab and a wearable-technology expert. “With the home monitoring enabled by these sensors, we can intervene at the right time, which could lead to better, faster recoveries for patients.”

(credit: Elliott Abel/ Shirley Ryan AbilityLab)
Monitoring movements, not sounds. The new band-aid-like stretchable throat sensor (two are applied) measures speech patterns by detecting throat movements to improve diagnosis and treatment of aphasia, a communication disorder associated with stroke.
Speech-language pathologists currently use microphones to monitor patients’ speech functions, which can’t distinguish between patients’ voices and ambient noise.

(credit: Elliott Abel/ Shirley Ryan AbilityLab)
Full-body kinematics. AbilityLab also uses similar electronic biosensors (developed in Rogers’ lab) on the legs, arms and chest to monitor stroke patients’ recovery progress. The sensors stream data wirelessly to clinicians’ phones and computers, providing a quantitative, full-body picture of patients’ advanced physical and physiological responses in real time.
Patients can wear them even after they leave the hospital, allowing doctors to understand how their patients are functioning in the real world.
(credit: Elliott Abel/ Shirley Ryan AbilityLab)
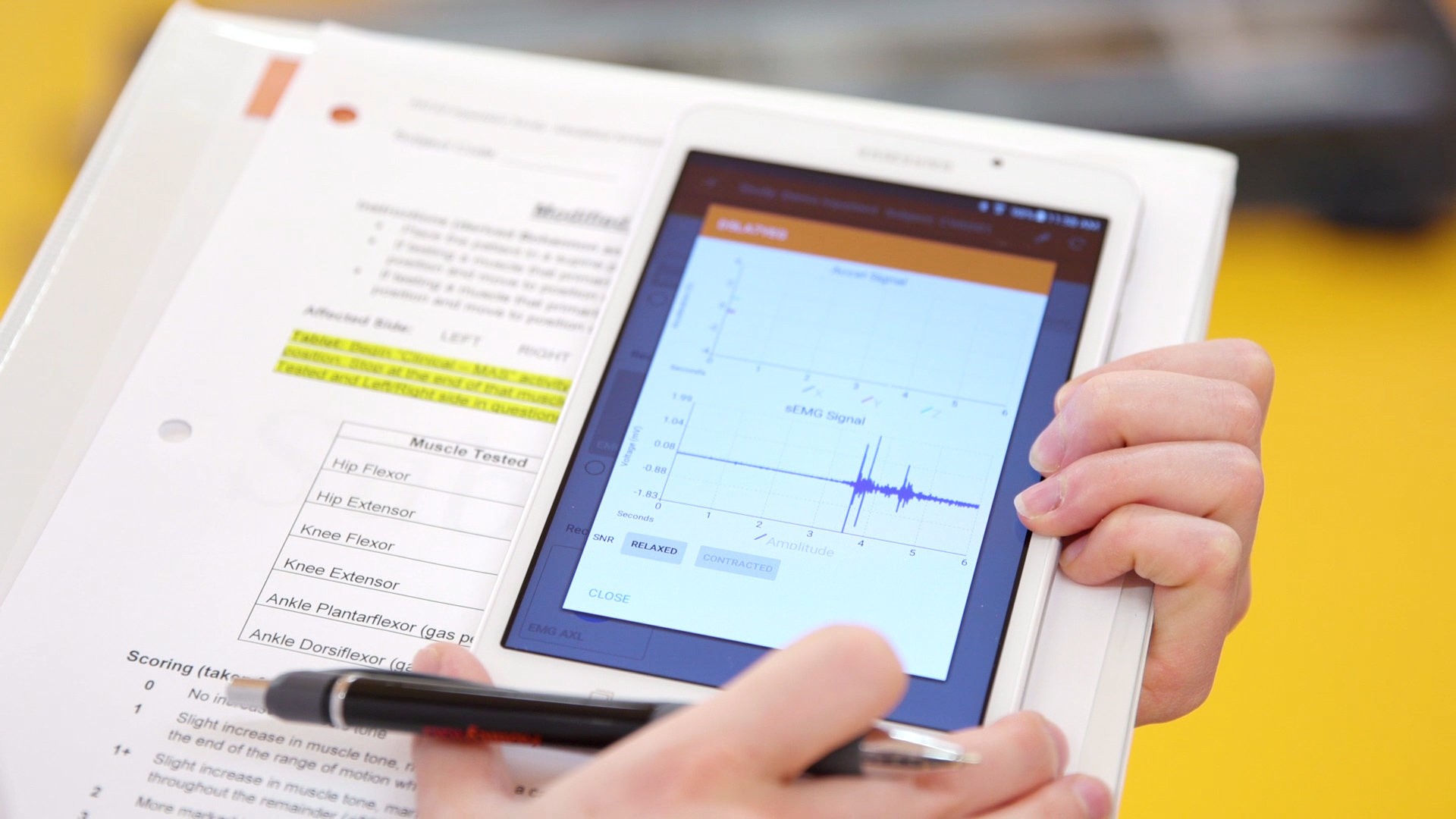
Mobile displays. Data from the sensors will be presented in a simple iPad-like display that is easy for both clinicians and patients to understand. It will send alerts when patients are under-performing on a certain metric and allow them to set and track progress toward their goals. A smartphone app can also help patients make corrections.
The researchers plan to test the sensors on patients with other conditions, such as Parkinson’s disease.

(credit: Elliott Abel/ Shirley Ryan AbilityLab)
Body-chemicals sensor. Another patch developed by the Rogers Lab does colorimetric analysis — determining the concentration of a chemical — for measuring sweat rate/loss and electrolyte loss. The Rogers Lab has a contract with Gatorade, and is testing this technology with the U.S. Air Force, the Seattle Mariners, and other unnamed sports teams.
Phone apps will also be available to capture precise colors and for data extraction, using algorithms.
A wearable electrocardiogram
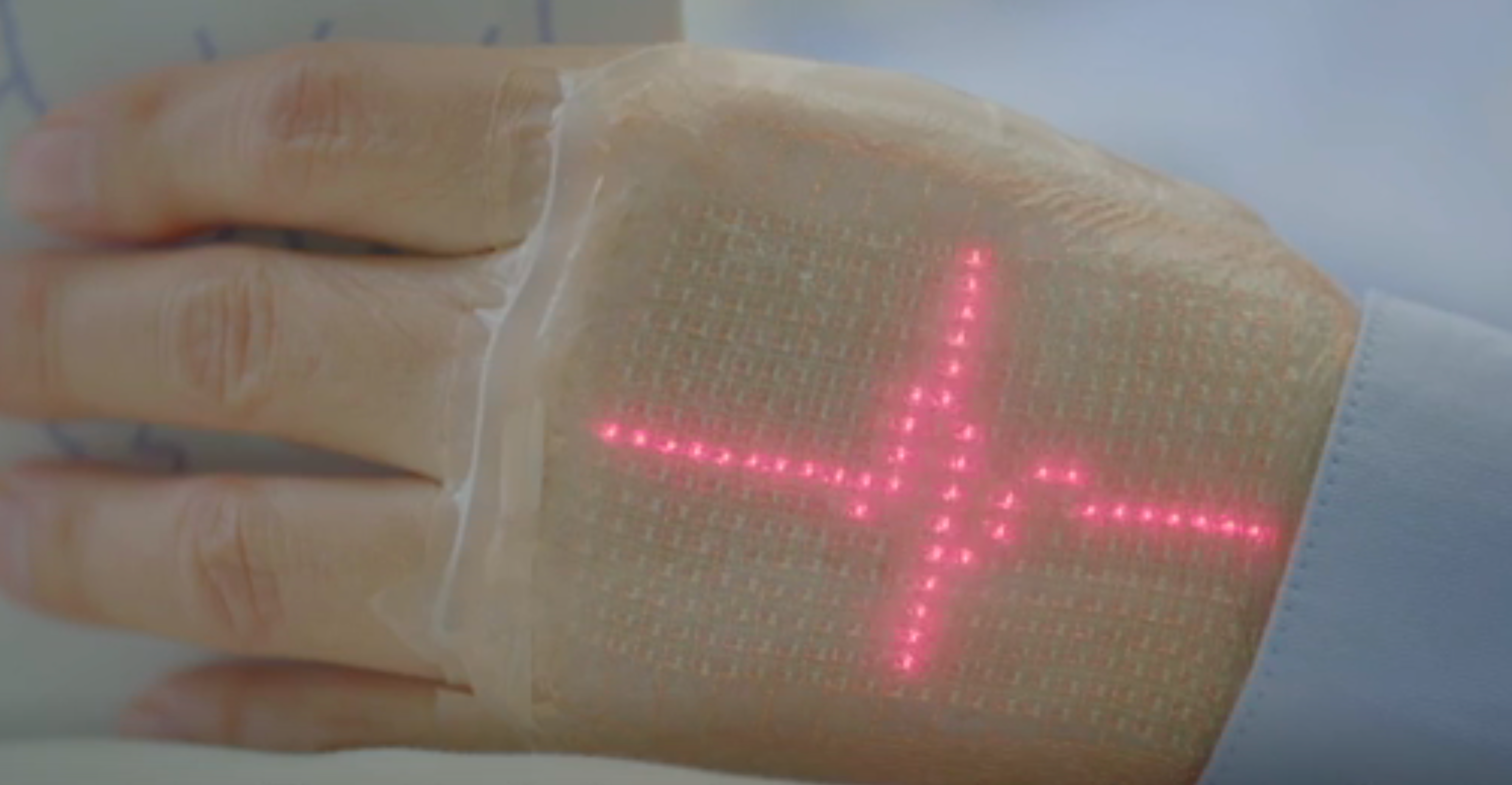
Electrocardiogram on a prototype skin sensor (credit: 2018 Takao Someya Research Group)
Wearing your heart of your sleeve. Imagine looking at a electrocardiogram displayed on your wrist, using a simple skin sensor (replacing the usual complex array of EKG body electrodes), linked wirelessly to a smartphone or the cloud.
That’s the concept for a new wearable device developed by a team headed by Professor Takao Someya at the University of Tokyo’s Graduate School of Engineering and Dai Nippon Printing (DNP). It’s designed to provide continuous, non-invasive health monitoring.
The soft, flexible skin display is about 1 millimeter thick. (credit: 2018 Takao Someya Research Group.)
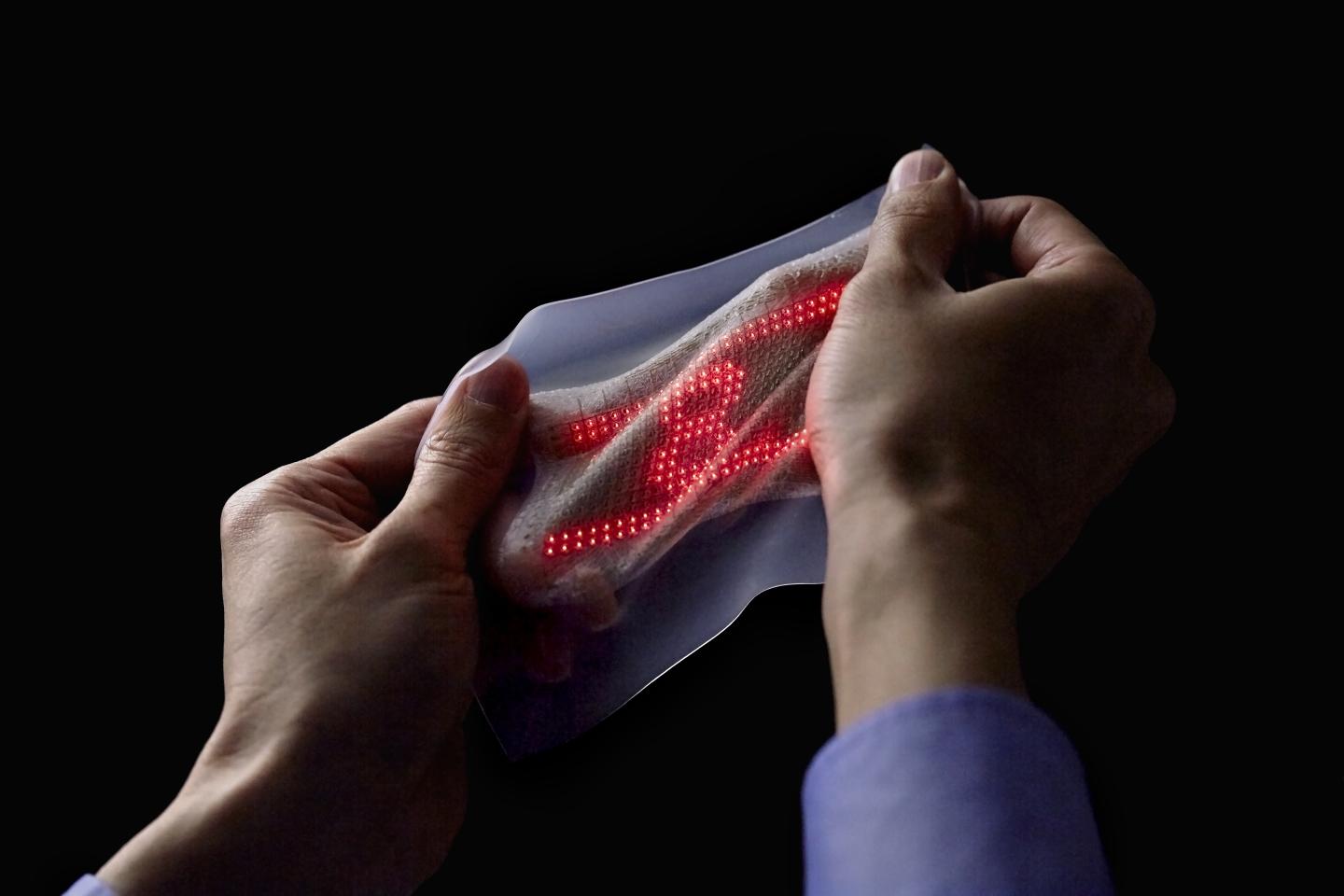
Stretchable nanomesh. The device uses a lightweight sensor made from a nanomesh electrode and a display made from a 16 x 24 array of micro LEDs and stretchable wiring, mounted on a rubber sheet. It’s stretchable by up 45 percent of its original length and can be worn on the skin continuously for a week without causing inflammation.
The sensor can also measure temperature, pressure, and the electrical properties of muscle, and can display messages on skin.
DNP hopes to bring the integrated skin display to market within three years.