Wireless brain stimulation with magnetic nanoparticles
March 15, 2015
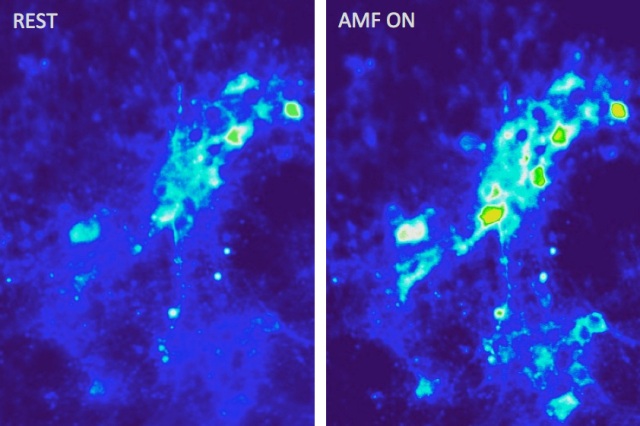
Images show calcium ion influx (right) into neurons as a result of magnetothermal excitation with alternating magnetic fields in the presence of magnetic nanoparticles (credit: MIT)
MIT researchers have developed a method to stimulate brain tissue using external magnetic fields and injected magnetic nanoparticles to treat neurological diseases such as Parkinson’s disease.
Currently, brain stimulation uses pulses of electricity and requires a surgically implanted electrode wired to a power source outside the brain.
In their study, the team injected magnetic iron oxide particles 22 nanometers in diameter into the brain.
When exposed to a low-frequency (100 kHz — 1 MHz) external alternating magnetic field —- which can penetrate deep inside biological tissues — these particles rapidly heat up.
The resulting local temperature increase can then lead to neural activation by triggering heat-sensitive capsaicin receptors -— the same proteins that the body uses to detect both actual heat and the “heat” of spicy foods. (Capsaicin is the chemical that gives hot peppers their searing taste.)
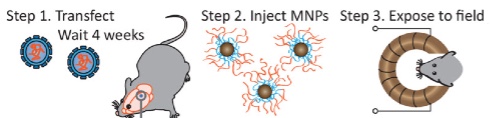
Wireless magnetothermal stimulation: in vivo experimental scheme (credit: Ritchie Chen et al./Science)
A team led by Polina Anikeeva, an assistant professor of materials science and engineering, used viral gene delivery to selected neurons in the brain to induce their sensitivity to heat.
The particles, which have virtually no interaction with biological tissues except when heated, tend to remain where they’re placed, allowing for long-term treatment without the need for further invasive procedures.
“The nanoparticles integrate into the tissue and remain largely intact,” Anikeeva says. “Then, that region can be stimulated at will by externally applying an alternating magnetic field.
MIT | Wireless brain stimulation
The new work has proven that the approach is feasible, but much work remains to turn this proof-of-concept into a practical method for brain research or clinical treatment.
Adapting cancer research with heated ferromagnetic particles
The use of magnetic fields and injected particles has been an active area of cancer research with the aim of destroying cancer cells by heating them. “The new technique is derived, in part, from that research,” Anikeeva says. “By calibrating the delivered thermal dosage, we can excite neurons without killing them. The magnetic nanoparticles also have been used for decades as contrast agents in MRI scans, so they are considered relatively safe in the human body.”
The team developed ways to make the particles with precisely controlled sizes and shapes to maximize their interaction with the applied alternating magnetic field. They also developed devices to deliver the applied magnetic field. Existing devices for cancer treatment — intended to produce much more intense heating — were far too big and energy-inefficient for this application.
The next step toward making this a practical technology for clinical use in humans “is to understand better how our method works through neural recordings and behavioral experiments, and assess whether there are any other side effects to tissues in the affected area,” Anikeeva says.
The research has been published in the journal Science. The work was funded by the Defense Advanced Research Projects Agency, MIT’s McGovern Institute for Brain Research, and the National Science Foundation.
Abstract of Wireless magnetothermal deep brain stimulation
Wireless deep brain stimulation of well-defined neuronal populations could facilitate the study of intact brain circuits and the treatment of neurological disorders. Here we demonstrate minimally-invasive and remote neural excitation through the activation of the heat-sensitive capsaicin receptor TRPV1 by magnetic nanoparticles. When exposed to alternating magnetic fields, the nanoparticles dissipate heat generated by hysteresis, triggering widespread and reversible firing of TRPV1+ neurons. Wireless magnetothermal stimulation in the ventral tegmental area of mice evoked excitation in subpopulations of neurons in the targeted brain region and in structures receiving excitatory projections. The nanoparticles persisted in the brain for over a month, allowing for chronic stimulation without the need for implants and connectors.