33 blood-cancer patients have dramatic clinical remission with new T-cell therapy
June 7, 2017
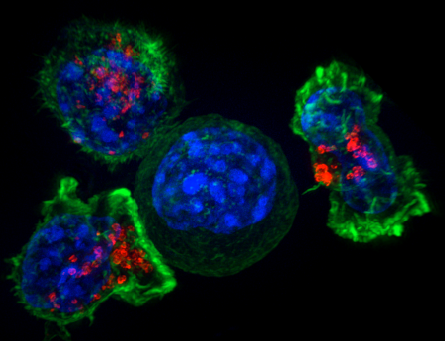
Image of a group of killer T cells (green and red) surrounding a cancer cell (blue, center) (credit: NIH)
Chinese doctors have reported success with a new type of immunotherapy for multiple myeloma*, a blood cancer: 33 out of 35 patients in a clinical trial had clinical remission within two months.
The researchers used a type of T cell called “chimeric antigen receptor (CAR) T.”** In a phase I clinical trial in China, the patient’s own T cells were collected, genetically reprogrammed in a lab, and injected back into the patient. The reprogramming involved inserting an artificially designed gene into the T-cell genome, which helped the genetically reprogrammed cells find and destroy cancer cells throughout the body.
The study was presented Monday (June 5, 2017) at the American Society of Clinical Oncology (ASCO) conference in Chicago.
“Although recent advances in chemotherapy have prolonged life expectancy in multiple myeloma, this cancer remains incurable,” said study author Wanhong Zhao, MD, PhD, an associate director of hematology at The Second Affiliated Hospital of Xi’an Jiaotong University in Xi’an, China. “It appears that with this novel immunotherapy there may be a chance for cure in multiple myeloma, but we will need to follow patients much longer to confirm that.”***
U.S. clinical trial planned
“While it’s still early, these data are a strong sign that CAR T-cell therapy can send multiple myeloma into remission,” said ASCO expert Michael S. Sabel, MD, FACS. “It’s rare to see such high response rates, especially for a hard-to-treat cancer. This serves as proof that immunotherapy and precision medicine research pays off. We hope that future research builds on this success in multiple myeloma and other cancers.”
The researchers plan to enroll a total of 100 patients in this continuing clinical trial at four participating hospitals in China. “In early 2018 we also plan to launch a similar clinical trial in the United States. Looking ahead, we would also like to explore whether BCMA CAR T-cell therapy benefits patients who are newly diagnosed with multiple myeloma,” said Zhao.
This study was funded by Legend Biotech Co.
* Multiple myeloma is a cancer of plasma cells, which make antibodies to fight infections. Abnormal plasma cells can crowd out or suppress the growth of other cells in the bone marrow. This suppression may result in anemia, excessive bleeding, and a decreased ability to fight infection. Multiple myeloma is a relatively uncommon cancer. This year, an estimated 30,300 people [Ref. 2] in the United States will be diagnosed with multiple myeloma, and 114,250 [Ref. 3] were diagnosed with this cancer worldwide in 2012. In the United States, only about half of patients survive five years after being diagnosed with multiple myeloma. — American Society of Clinical Oncology
** Over the past few years, CAR T-cell therapy targeting a B-cell biomarker called CD19 proved very effective in initial trials for acute lymphoblastic leukemia (ALL) and some types of lymphoma, but until now, there has been little success with CAR T-cell therapies targeting other biomarkers in other types of cancer. This is one of the first clinical trials of CAR T cells targeting BCMA, which was discovered to play a role in progression of multiple myeloma in 2004. — American Society of Clinical Oncology
*** To date, 19 patients have been followed for more than four months, a pre-set time for full efficacy assessment by the International Myeloma Working Group (IMWG) consensus. Of the 19 patients, 14 have reached stringent complete response (sCR) criteria, one patient has reached partial response, and four patients have achieved very good partial remission (VgPR) criteria in efficacy. There has been only a single case of disease progression from VgPR; an extramedullary lesion of the VgPR patient reappeared three months after disappearing on CT scans. There has not been a single case of relapse among patients who reached sCR criteria. The five patients who have been followed for over a year (12–14 months) all remain in sCR status and are free of minimal residual disease as well (have no detectable cancer cells in the bone marrow). Cytokine release syndrome or CRS, a common and potentially dangerous side effect of CAR T-cell therapy, occurred in 85% of patients, but it was only transient. In the majority of patients symptoms were mild and manageable. CRS is associated with symptoms such as fever, low blood pressure, difficulty breathing, and problems with multiple organs. Only two patients on this study experienced severe CRS (grade 3) but recovered upon receiving tocilizumab (Actemra, an inflammation-reducing treatment commonly used to manage CRS in clinical trials of CAR T-cell therapy). No patients experienced neurologic side effects, another common and serious complication from CAR T-cell therapy. — American Society of Clinical Oncology
Abstract of Durable remissions with BCMA-specific chimeric antigen receptor (CAR)-modified T cells in patients with refractory/relapsed multiple myeloma.
Background: Chimeric antigen receptor engineered T cell (CAR-T) is a novel immunotherapeutic approach for cancer treatment and has been clinically validated in the treatment of acute lymphoblastic leukemia (ALL). Here we report an encouraging breakthrough of treating multiple myeloma (MM) using a CAR-T designated LCAR-B38M CAR-T, which targets principally BCMA. Methods: A single arm clinical trial was conducted to assess safety and efficacy of this approach. A total of 19 patients with refractory/relapsed multiple myeloma were included in the trial. The median number of infused cells was 4.7 (0.6 ~ 7.0) × 10e6/ kg. The median follow-up times was 208 (62 ~ 321) days. Results: Among the 19 patients who completed the infusion, 7 patients were monitored for a period of more than 6 months. Six out of the 7 achieved complete remission (CR) and minimal residual disease (MRD)-negative status. The 12 patients who were followed up for less than 6 months met near CR criteria of modified EBMT criteria for various degrees of positive immunofixation. All these effects were observed with a progressive decrease of M-protein and thus expected to eventually meet CR criteria. In the most recent follow-up examination, all 18 survived patients were determined to be free of myeloma-related biochemical and hematologic abnormalities. One of the most common adverse event of CAR-T therapy is acute cytokine release syndrome (CRS). This was observed in 14 (74%) patients who received treatment. Among these 14 patients there were 9 cases of grade 1, 2 cases of grade 2, 1 case of grade 3, and 1 case of grade 4 patient who recovered after treatments. Conclusions: A 100% objective response rate (ORR) to LCAR-B38M CAR-T cells was observed in refractory/relapsed myeloma patients. 18 out of 19 (95%) patients reached CR or near CR status without a single event of relapse in a median follow-up of 6 months. The majority (14) of the patients experienced mild or manageable CRS, and the rest (5) were even free of diagnosable CRS. Based on the encouraging safety and efficacy outcomes, we believe that our LCAR-B38M CAR-T cell therapy is an innovative and highly effective treatment for multiple myeloma.