A potential breakthrough in using electrical pulses to treat deadly glioblastoma brain tumors
February 20, 2015
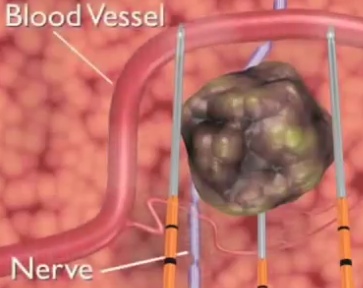
Irreversible electroporesis destroys a cerebral lesion while leaving nearby important vessels and organs unharmed (credit: URMC)
Based on successful results in an experiment with a Labrador retriever using a novel treatment for glioblastoma brain cancer, the National Cancer Institute yesterday (Feb. 19) awarded Scott Verbridge, an assistant professor of biomedical engineering and mechanics at Virginia Tech , a $386,149 research grant to take a related medical procedure a step closer to using on humans.
The team’s findings from the experiment were reported in an open-access paper in the Feb. 14, 2011, issue of the Journal of Technology Cancer Research and Treatment.
Since the surgery, the investigators have continued experiments and mathematical modeling techniques that are leading toward effective treatments for humans with glioblastoma, the most common and deadly malignant brain tumor.
Punching holes in a tumor
The technique, invented by Virginia Tech faculty member Rafael Davalos, is called irreversible electroporation (basically, punching tiny holes in cancer tissue with electricity).
The investigators propose in the current project that these pulses can be tuned “to target the unique physical properties of malignant cells,” Verbridge said.
By contrast, chemotherapy and radiation used to reduce or eliminate cancerous cells are not discriminatory and can also affect healthy cells.
Clinical trials using the irreversible electroporation procedure have also been conducted for treatment of liver, kidney, pancreatic, and lung cancer.
“The procedure is essentially done with two minimally invasive electrodes placed into the targeted region, delivering approximately 80 pulses to the site in about one minute. The pulses are high voltage but low energy, so no significant heating occurs as a result of the procedure,” Davalos said. They use a device called Nanoknife for that purpose.
AngioDynamics® | URMC introduces NanoKnife technology for soft-tissue tumors
Pulse duration is significant in this process. Earlier studies have demonstrated that length of the pulse accounts for the dead cell lesion size, and the current work will explore the impact of varying these time parameters on the response of different cell types within gliomas.
In addition to researching the response of cell lines, experiments also will include patient-derived cells harvested by colleagues at Wake Forest University and The Ohio State University Comprehensive Cancer Centers. The researchers plan to build three-dimensional in vitro tumors using these patient-derived cells.
They then will characterize the response of the most highly aggressive tumor cell populations, in physiologically relevant tissue models, to these electric field therapies. Using live staining techniques and confocal microscopy, the researchers will be able to measure real-time responses of the cells to the irreversible electroporation.
“We believe our studies will provide a significant advancement in our understanding of glioma biology and point to new treatment possibilities,” said Verbridge, who conducted postdoctoral research at the National Institutes of Health (NIH)-funded Cornell University Physical Sciences in Oncology Center. Verbridge also is a principal investigator on an additional NIH-funded project investigating glioma transcriptional dynamics, in collaboration with Chang Lu of Virginia Tech’s Department of Chemical Engineering.
Abstract for Non-thermal irreversible electroporation (N-TIRE) and adjuvant fractionated radiotherapeutic multimodal therapy for intracranial malignant glioma in a canine patient
Non-thermal irreversible electroporation (N-TIRE) has shown promise as an ablative therapy for a variety of soft-tissue neoplasms. Here we describe the therapeutic planning aspects and first clinical application of N-TIRE for the treatment of an inoperable, spontaneous malignant intracranial glioma in a canine patient. The N-TIRE ablation was performed safely, effectively reduced the tumor volume and associated intracranial hypertension, and provided sufficient improvement in neurological function of the patient to safely undergo adjunctive fractionated radiotherapy (RT) according to current standards of care. Complete remission was achieved based on serial magnetic resonance imaging examinations of the brain, although progressive radiation encephalopathy resulted in the death of the dog 149 days after N-TIRE therapy. The length of survival of this patient was comparable to dogs with intracranial tumors treated via standard excisional surgery and adjunctive fractionated external beam RT. Our results illustrate the potential benefits of N-TIRE for in vivo ablation of undesirable brain tissue, especially when traditional methods of cytoreductive surgery are not possible or ideal, and highlight the potential radiosensitizing effects of N-TIRE on the brain.