3D-printed sensors to lower cost, improve comfort in diabetes management
March 18, 2015
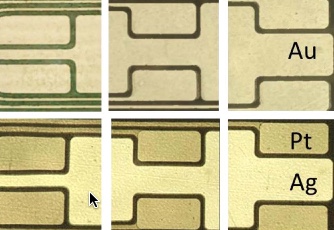
Optical microscopy images of patterned gold on polyimide film substrate (top) prepared via microcontact printing and after platinum and silver electrodes deposition (bottom) by electroplating (credit: Xiaosong Du et al./ Xiaosong Du/ ECS Journal of Solid State Science and Technology)
Engineers at Oregon State University have used additive manufacturing to create an improved type of glucose sensor for patients with Type 1 diabetes, part of a system that should work better, cost less, and be more comfortable for the patient.
A key advance is use of an electrohydrodynamic jet (“e-jet” printing) to make the sensor, which detects glucose concentration based on electric current flow. Conceptually, e-jet printing is a little like an inexpensive inkjet printer, but it creates much finer drop sizes and works with biological materials such as enzymes, instead of ink.
It uses a thin polyimide substrate that allows for wrapping the e-jet printed sensors around catheters with high radius of curvature.
The technology would create an “artificial pancreas” using a single point of bodily entry, or catheter, replacing existing systems, which require four entry points, usually packaged in a belt worn around the waist, according to Greg Herman, an OSU associate professor of chemical engineering.
“This technology and other work that could evolve from it should improve a patient’s health, comfort and diabetes management,” said Herman.
Diabetes management systems provide constant monitoring of blood glucose concentrations and are matched with portable infusion pumps. They control delivery of the hormones insulin and glucagon, and maintain safe levels of glucose in the blood.
The findings were reported in an open-access paper in the ECS Journal of Solid State Science and Technology.
Type 1 diabetes, previously called “juvenile diabetes,” can lead to serious health complications unless glucose levels are carefully controlled. Problems can include retinopathy, blindness, neuropathy, and kidney and cardiac disease.
The researchers say that this system may ultimately prove useful with Type 2 diabetes as well, and that it has the capability of making other biological measurements in addition to blood sugar.
More precise, compact, less intrusive, lower-cost
From an engineering perspective, the new approach is more precise, less intrusive, uses fewer processing steps, avoids waste and costs less.
“These are disposable devices that only last about a week and then need to be replaced,” Herman said. “Some other approaches used to make them might waste up to 90 percent of the materials being used, and that’s a problem in a throw-away sensor. It’s also important to keep costs as low as possible, and printing systems are inherently low-cost.”
Another important advance was the use of plastic (polyimide) substrates, which are the same thickness as kitchen plastic wrap, so that the sensors can be wrapped around a catheter.
“The challenges of making these sensors on such thin plastic films were difficult to overcome, but we found that additive manufacturing approaches simplified the process, and should lead to much lower costs,” said John Conley, an OSU professor of electrical engineering.
A patent has been applied for on the technology by OSU and Pacific Diabetes Technologies of Portland, Ore., which is working to commercialize the system. It’s already being tested in animals, and there are no apparent obstacles to its development in the health marketplace, Herman said.
Collaborators on the research included the Oregon Health & Science University and Pacific Diabetes Technologies. Support came from the National Institutes of Health, the Leona M. and Harry B. Helmsley Charitable Trust, the Oregon Nanoscience and Microtechnologies Institute, and the Juvenile Diabetes Research Foundation.
Diabetes is a global, rapidly increasing health problem. In 2014, the International Diabetes Federation estimated that 387 million people around the world had some type of diabetes, and that number is expected to rise to 592 million within 20 years. The global economic cost last year was estimated at $612 billion, and the agency reported that more than three out of four people with diabetes live in low or middle-income countries.
Abstract of Fabrication of a Flexible Amperometric Glucose Sensor Using Additive Processes
This study details the use of printing and other additive processes to fabricate a novel amperometric glucose sensor. The sensor was fabricated using a Au coated 12.7 μm thick polyimide substrate as a starting material, where micro-contact printing, electrochemical plating, chloridization, electrohydrodynamic jet (e-jet) printing, and spin coating were used to pattern, deposit, chloridize, print, and coat functional materials, respectively. We have found that e-jet printing was effective for the deposition and patterning of glucose oxidase inks with lateral feature sizes between ∼5 to 1000 μm in width, and that the glucose oxidase was still active after printing. The thickness of the permselective layer was optimized to obtain a linear response for glucose concentrations up to 32 mM and no response to acetaminophen, a common interfering compound, was observed. The use of such thin polyimide substrates allow wrapping of the sensors around catheters with high radius of curvature ∼250 μm, where additive and microfabrication methods may allow significant cost reductions.