Bionic eye clinical trial results: long-term safety, efficacy
June 24, 2015
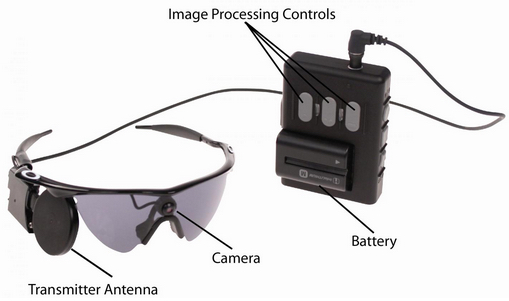
The external components of the Argus II System. Images in real time are captured by camera mounted on the glasses. The video processing unit down-samples and processes the image, converting it to retinal-stimulation patterns. Data and power are sent via radio frequency link from the transmitter antenna on the glasses to the receiver antenna around the eye (see illustration below). A removable, rechargeable battery powers the system. (credit: Second Sight Medical Products, Inc.)
Three-year clinical trial results of the Argus II retinal implant (“bionic eye”) have found that the device restored some visual function and quality of life for 30 people blinded by retinitis pigmentosa, a rare degenerative eye disease. The findings, published in an open-access paper in the journal Ophthalmology, also showed long-term efficacy, safety and reliability for the device.
Retinitis pigmentosa is an incurable disease that affects about 1 in 4,000 Americans and causes slow vision loss that eventually leads to blindness.
Using the Argus II, patients are able to see patterns of light that the brain learns to interpret as an image. The system uses a miniature video camera connected to the glasses to send visual information to a small computerized video processing unit and battery that can be stored in a pocket. This computer turns the image to electronic signals that are sent wirelessly to an electronic device surgically implanted on the retina in the eye.
The Argus II received FDA approval as a Humanitarian Use Device (HUD) in 2013 and in Europe Argus II received the CE Mark in 2011 and was launched commercially in Italy, Germany, France, Spain, The Netherlands, Switzerland and England.
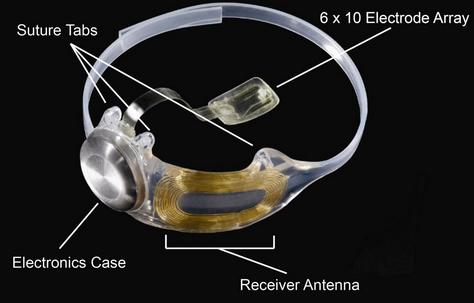
The implanted portions of the Argus II System (credit: Second Sight Medical Products, Inc.)
The clinical trial was conducted in the United States and Europe. All of the study participants had little or no light perception in both eyes.
Test results: a viable treatment option
The researchers conducted two visual-function tests using both a computer screen and real-world conditions: finding and touching a door and identifying and following a line on the ground. A Functional Low-vision Observer Rated Assessment (FLORA) was also performed by independent visual rehabilitation experts at the request of the FDA to assess the impact of the Argus II system on the subjects’ everyday lives, including extensive interviews and tasks performed around the home.
The visual function results indicated that up to 89 percent of the subjects performed significantly better with the device. The FLORA found that among the subjects, 80 percent received benefit from the system when considering both functional vision and patient-reported quality of life, and no subjects were affected negatively.
After one year, two-thirds of the subjects had not experienced device- or surgery-related serious adverse events. After three years, there were no device failures. Throughout the three years, 11 subjects experienced serious adverse events, most of which occurred soon after implantation and were successfully treated. One of these treatments, however, was to remove the device due to recurring erosion after the suture tab on the device became damaged.
“This study shows that the Argus II system is a viable treatment option for people profoundly blind due to retinitis pigmentosa – one that can make a meaningful difference in their lives and provides a benefit that can last over time,” said Allen C. Ho, M.D., lead author of the study and director of the clinical retina research unit at Wills Eye Hospital.
The Argus II has 60 electrodes (pixels), which limits it to relatively large objects. There are higher-resolution devices in development. Retina Implant’s Alpha IMS Subretinal Microchip is a 1,500-pixel chip (no external video camera required). And Stanford University photovoltaic subretinal prosthesis research project achieves 178 pixels per square millimeter, scalable to thousands of pixels. Silicon photodiodes in each pixel directly convert pulsed near-infrared (NIR) images projected from video goggles, eliminating a hard-wire connection.
Abstract of Long-Term Results from an Epiretinal Prosthesis to Restore Sight to the Blind
Purpose: Retinitis pigmentosa (RP) is a group of inherited retinal degenerations leading to blindness due to photoreceptor loss. Retinitis pigmentosa is a rare disease, affecting only approximately 100 000 people in the United States. There is no cure and no approved medical therapy to slow or reverse RP. The purpose of this clinical trial was to evaluate the safety, reliability, and benefit of the Argus II Retinal Prosthesis System (Second Sight Medical Products, Inc, Sylmar, CA) in restoring some visual function to subjects completely blind from RP. We report clinical trial results at 1 and 3 years after implantation.
Design: The study is a multicenter, single-arm, prospective clinical trial.
Participants: There were 30 subjects in 10 centers in the United States and Europe. Subjects served as their own controls, that is, implanted eye versus fellow eye, and system on versus system off (native residual vision).
Methods: The Argus II System was implanted on and in a single eye (typically the worse-seeing eye) of blind subjects. Subjects wore glasses mounted with a small camera and a video processor that converted images into stimulation patterns sent to the electrode array on the retina.
Main Outcome Measures: The primary outcome measures were safety (the number, seriousness, and relatedness of adverse events) and visual function, as measured by 3 computer-based, objective tests.
Results: A total of 29 of 30 subjects had functioning Argus II Systems implants 3 years after implantation. Eleven subjects experienced a total of 23 serious device- or surgery-related adverse events. All were treated with standard ophthalmic care. As a group, subjects performed significantly better with the system on than off on all visual function tests and functional vision assessments.
Conclusions: The 3-year results of the Argus II trial support the long-term safety profile and benefit of the Argus II System for patients blind from RP. Earlier results from this trial were used to gain approval of the Argus II by the Food and Drug Administration and a CE mark in Europe. The Argus II System is the first and only retinal implant to have both approvals.