Cell-detection system promising for medical research, diagnostics
October 10, 2013
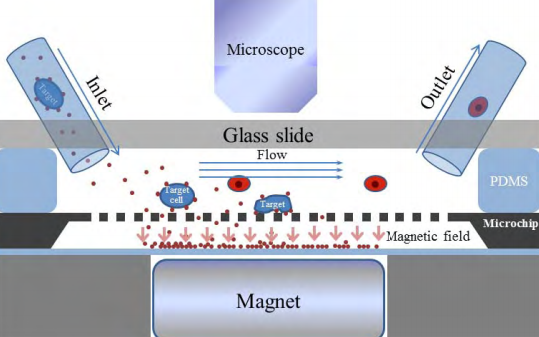
This schematic depicts a new system that uses tiny magnetic beads to quickly detect rare types of cancer cells circulating in a patient’s blood (credit: Bin-Da Chan/Purdue School of Mechanical Engineering)
Researchers are developing a system that uses tiny magnetic beads to quickly detect rare types of cancer cells circulating in a patient’s blood, an advance that could help medical doctors diagnose cancer earlier than now possible and monitor how well a patient is responding to therapy.
While other researchers have used magnetic beads for similar applications, the new “high-throughput” system has the ability to quickly process and analyze large volumes of blood or other fluids, said Cagri Savran (pronounced Chary Savran), an associate professor of mechanical engineering at Purdue University.
He is working with oncologists at the Indiana University School of Medicine to further develop the technology, which recently was highlighted in the journal Lab on a Chip.
The approach combines two techniques: immunomagnetic separation and microfluidics.
In immunomagnetic separation, magnetic beads about a micron in diameter are “functionalized,” or coated with antibodies that recognize and attach to antigens on the surface of target cells.
The researchers functionalized the beads to recognize breast cancer and lung cancer cells in laboratory cultures.
“We were able to detect cancer cells with up to a 90 percent yield,” said Savran, working with Purdue postdoctoral fellow Chun-Li Chang and medical researchers Shadia Jalal and Daniela E. Matei from the IU School of Medicine’s Department of Medicine. “We expect this system to be useful in a wide variety of settings, including detection of rare cells for clinical applications.”
Previous systems using immunomagnetic separation to isolate cells required that the cells then be transferred to another system to be identified, counted and studied.
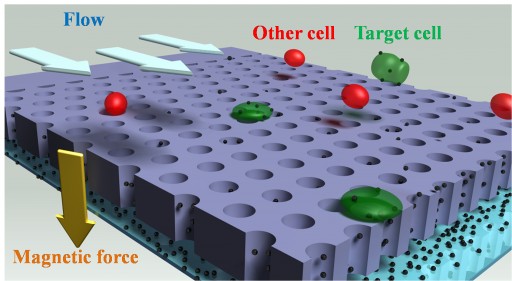
“What’s new here is that we’ve built a system that can perform all of these steps on one chip,” said Savran, also an associate professor of biomedical engineering. “It both separates cells and also places them on a chip surface so you can count them and study them with a microscope.”
Another innovation is the fast processing, he said. Other “microfluidic” chips are unable to quickly process large volumes of fluid because they rely on extremely narrow channels, which restrict fluid flow.
“The circulating cancer cells are difficult to detect because very few of them are contained in blood,” Savran said. “That means you have to use as many magnetic beads as practically possible to quickly screen and process a relatively large sample, or you won’t find these cells.”
The new design passes the fluid through a chamber that allows for faster flow; a standard 7.5-milliliter fluid sample can run through the system in a matter of minutes.
The beads are directed by a magnetic field to a silicon mesh containing holes 8 microns in diameter. Because the target cells are so sparse, many of the beads fail to attract any and pass through the silicon mesh. The beads that have attached to cells are too large to pass through the holes in the mesh.
If needed, the cells can quickly be flushed from the system for further analysis simply by turning off the magnetic field.
“Not only can the cells be readily retrieved for further usage, the chip can be re-used for subsequent experiments,” Savran said.
The technology also could be used to cull other types of cells.
“This is not only for cancer applications,” he said.
The work has been supported by the Walther Oncology Physical Sciences and Engineering Research Embedding Program in the Purdue Oncological Sciences Center, the Purdue Center for Cancer Research, the National Science Foundation and the Indiana University Melvin and Bren Simon Cancer Center.
Abstract of Lab on a Chip paper
We report a microchip system based on a combination of immunomagnetic separation and microfluidics for high-throughput detection of whole cells. In this system target cells bound to magnetic beads flow parallel to a microchip with flow rates of mLs/min. A magnetic field draws the bead-bound cells toward the microchip, which contains apertures that allow passage of unbound beads while trapping the target cells. The cells can be analyzed clearly under a microscope and released from the chip for further analysis by removing the magnetic field. The system was characterized by detecting breast cancer cells (MCF-7) and lung cancer cells (A549) in culture media using anti-EpCAM conjugated magnetic beads. We were able to detect MCF-7 cells with > 90% yield using a flow rate of about 4 mL/min, and A549 cells with 78% yield with 1 mL/min. We also demonstrated high-throughput detection of cells with concentrations as low as 0.8 cells/mL in large sample volumes (12 mL). We expect this system to be useful in a wide variety of settings, including detection of rare cells for clinical applications.