Heated nanoparticles trigger immune systems deactivated by cancer
October 10, 2014
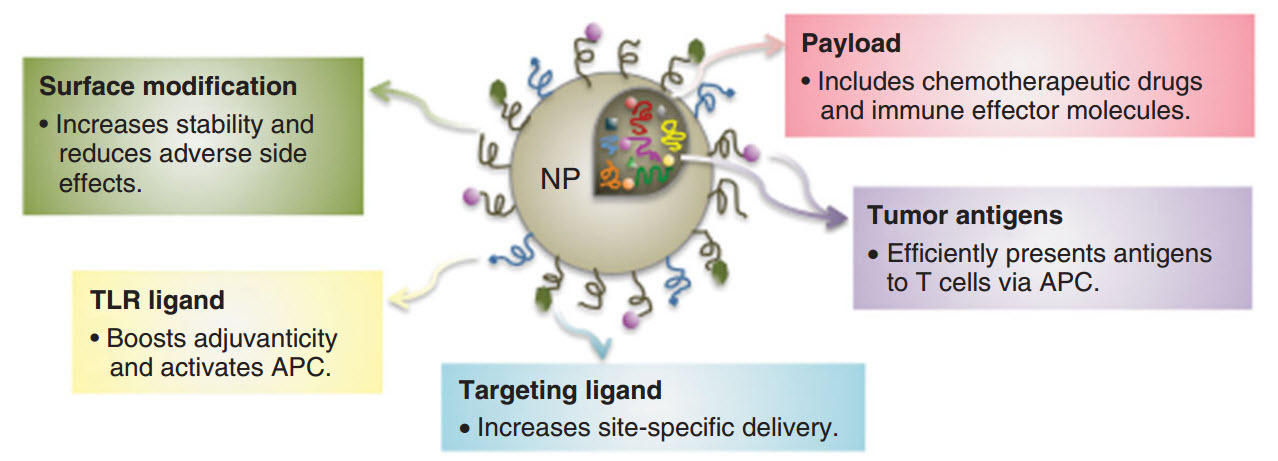
Schematic diagram of types of nanoparticle (NP) platforms for therapeutic applications, including external “weapons” (surface modification, toll-like receptor (TLR) ligands (linking molecules) that activate antigen-presenting cells (APCs) and targeting ligands); and stealth methods — tumor-antigen load and payload composed of therapeutic entities (credit: Mee Rie Sheen, Patrick H. Lizotte, Seiko Toraya‐Brown, Steven Fiering/WIREs Nanomedicine and Nanobiotechnology)
Researchers at Dartmouth-Hitchcock Norris Cotton Cancer Center have developed a method to use heat with nanoparticles to wake up the immune system so it recognizes and attacks invading cancer cells, according to Steve Fiering, PhD, Norris Cotton Cancer Center researcher and professor of Microbiology and Immunology, and of Genetics at the Geisel School of Medicine at Dartmouth.
The innovation uses a well-known method of killing cancer cells: a metallic nanoparticle containing iron, silver, or gold injected into the cancer cell and then heated externally, using magnetic energy, infrared light, or radio waves;
But that method can’t kill all of the resilient cancer cells. What’s new is the use of heat to trigger the immune system to attack cancer cells — overcoming a tactic used by cancer cells to protect themselves by tricking the immune system into accepting everything as normal, even while cancer cells are dividing and spreading.
Nanoparticles and tumor immunology
This is one of an expanding array of nanoparticle types discussed a review article on that discusses the confluence of two rapidly developing areas of cancer therapy, nanoparticles and tumor immunology, published in an issue of Wiley’s WIREs Nanomedicine and Nanobiotechnology. (KurzweilAI has also covered this in these news posts.)
Nanoparticles’ small size makes them stealthy enough to penetrate cancer cells with therapeutic agents such as antibodies, drugs, vaccine type viruses, or metallic particles, the authors explain. But nanoparticles can also pack large payloads of a variety of agents that have different effects that activate and strengthen the body’s immune-system response against tumors.
These approaches are still early in development in the laboratory or clinical trials. But “now that efforts to stimulate anti-tumor immune responses are moving from the lab to the clinic, the potential for nanoparticles to be utilized to improve an immune-based therapy approach is attracting a lot of attention from both scientists and clinicians. And clinical usage does not appear too distant,” said Fiering.
Abstract of WIREs Nanomedicine and Nanobiotechnology paper
A variety of strategies, have been applied to cancer treatment and the most recent one to become prominent is immunotherapy. This interest has been fostered by the demonstration that the immune system does recognize and often eliminate small tumors but tumors that become clinical problems block antitumor immune responses with immunosuppression orchestrated by the tumor cells. Methods to reverse this tumor-mediated immunosuppression will improve cancer immunotherapy outcomes. The immunostimulatory potential of nanoparticles (NPs), holds promise for cancer treatment. Phagocytes of various types are an important component of both immunosuppression and immunostimulation and phagocytes actively take up NPs of various sorts, so NPs are a natural system to manipulate these key immune regulatory cells. NPs can be engineered with multiple useful therapeutic features, such as various payloads such as antigens and/or immunomodulatory agents including cytokines, ligands for immunostimulatory receptors or antagonists for immunosuppressive receptors. As more is learned about how tumors suppress antitumor immune responses the payload options expand further. Here we review multiple approaches of NP-based cancer therapies to modify the tumor microenvironment and stimulate innate and adaptive immune systems to obtain effective antitumor immune responses.