How to create beating heart muscle cells
October 15, 2012
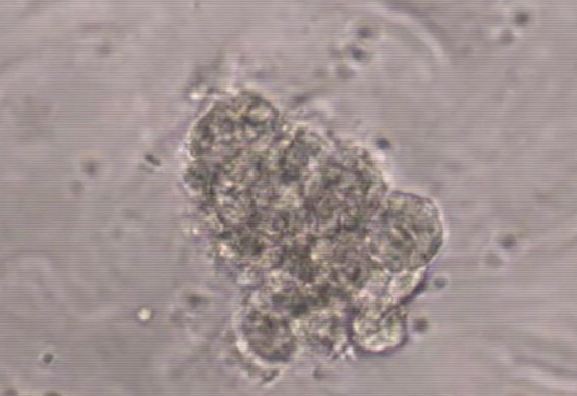
Explant cultures of Scl yolk sac plated on OP9 stroma produced individual beating cells already after 4 hours (from video; credit: UCLA)
UCLA stem-cell researchers have found for the first time a surprising and unexpected plasticity in the embryonic endothelium, the place where blood stem cells are made in early development.
They found that the lack of one transcription factor, a type of gene that controls cell fate (by regulating other genes), allows the precursors that normally generate blood stem and progenitor cells in blood-forming tissues to become something very unexpected — beating cardiomyocytes, or heart muscle cells.
The finding is important because it suggests that the endothelium can serve as a source of heart muscle cells. The finding may provide new understanding of how to make cardiac stem cells for use in regenerative medicine, said study senior author Dr. Hanna Mikkola, an associate professor of molecular, cell and developmental biology in Life Sciences and a researcher with the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA.
“It was absolutely unbelievable. These findings went beyond anything that we could have imagined,” Mikkola said. “The microenvironment in the embryonic vasculature that normally gives rise to blood cells can generate cardiac cells when only one factor, Scl, is removed, essentially converting a hematopoietic organ into a cardiogenic organ.”
The findings were so surprising, in fact, that Mikkola and her team did not want to believe the results until all subsequent assays proved the finding to be true, said Amelie Montel-Hagen, study co-first author and a post-doctoral fellow.
“To make sure we had not switched the samples between blood forming tissues and the heart we ran the experiments again and repeatedly got the same results,” Montel-Hagen said. “It turns out Scl acts as a conductor in the orchestra, telling the other genes in the endothelium who should be playing and who shouldn’t be playing.”
The team used microarray technology to determine which genes were “playing” in embryonic endothelium to generate blood stem and progenitor cells and found that in the absence of Scl, the genes required for making cardiomyocytes were activated instead, said study co-first author Ben Van Handel, a post-doctoral fellow.
“Scl has a known role as a master regulator of blood development and when we removed it from the equation, no blood cells were made,” Van Handel said. “That the removal of Scl resulted in fully functional cardiomyocytes in blood forming tissues was unprecedented.”
The team used the yolk sac — rhe first tissue where blood cells are made — from embryos that lacked Scl and within four hours of plating on the culture dish, the tissue had generated beating cardiomyocytes. The team also found similar cardiomyocyte potential in Scl-deficient embryos in the endocardium that lines the heart chambers. They also looked for genetic signatures that would suggest that these endothelial precursors could potentially also make other closely related tissues such as skeletal muscle, bone or kidney, but found no evidence of such plasticity. The default fate of the endothelium was to make cardiomyocytes in the absence of Scl, Mikkola said.
The findings may also have implications in cell reprogramming, which generally calls for adding factors to induce cell fate change, a process that can be problematic. It might be safer to suppress a factor like Scl to nudge cells into a cardiomyocyte fate, Mikkola said.
“This study opens new ways to think about what could be a potential source of cardiac stem cells,” she said. “We now have a better understanding of how cardiac progenitor cells can be made and regulated, and this may one day lead us to a way to treat heart attacks by creating new heart muscle cells to replace those that were damaged.”
Going forward, Mikkola and her team plan to investigate the developmental and regenerative potential of the endothelium-derived cardiac progenitor cells, and define the mechanisms by which Scl can at the same time activate one fate while suppressing another.
“These results call for future studies to examine the prospect of harnessing the latent cardiogenic potential in the vasculature for use in regenerative medicine, and to investigate whether similar development plasticity exists in other major cell fate decisions in the developing embryo,” the study states.
The study was funded by a California Institute of Regenerative Medicine New Faculty Award, a National Institutes of Health’s National Heart Lung and Blood Institute (RO1 HL097766-01), an Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA Innovation Award, a National Institutes of Health Ruth L. Kirschstein National Research Service Awards (GM07185 and T32 HL69766), the European Molecular Biology Organization, the Human Frontier Science Program, the Netherlands Organization for Scientific Research, European Social Fund (Mobilitas), and the Center of Excellence in Molecular Hematology from the National Institute of Diabetes and Digestive and Kidney Diseases.