Injecting glucose sugar makes cancer light up in MRI scanners
July 9, 2013
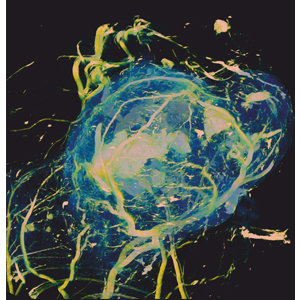
Tumors use large quantities of glucose to sustain their growth. Blood vessels supplying glucose to the tumor are shown here in yellow, with soft tissue surrounding them shown in blue. This image was acquired using micro-CT (computed tomography) at a resolution of 6 microns and was used to investigate a new biomedical imaging technique called glucoCEST, developed by UCL scientists as a way to detect its accumulation in tumors using magnetic resonance imaging (MRI). (Credit: University College London)
UCL scientists have developed a new technique for detecting cancer by imaging the uptake (consumption) of glucose sugar with magnetic resonance imaging (MRI).
The breakthrough could provide a safer and simpler alternative to x-ray radiation and enable radiologists to image tumors in greater detail.
The new technique, called “glucose chemical exchange saturation transfer” (glucoCEST), is based on the fact that to sustain their rapid growth, tumors consume much more glucose (a type of sugar) than normal healthy tissues. It can also distinguish tumor types with differing metabolic characteristics and pathophysiologies.
The method uses the chemical exchange of protons between hydroxyl groups and water.*
Imaging tumors with MRI
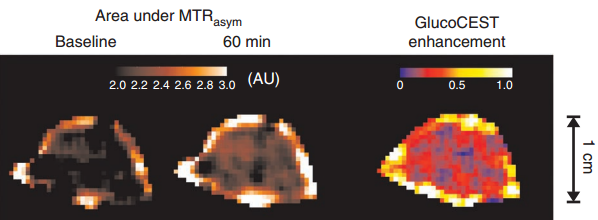
glucoCEST image data from a tumor showing images before and 60 min after injection of glucose solution. (credit: Simon Walker-Samuel et al./UCL/Nature Medicine)
The researchers found that sensitizing an MRI scanner to glucose uptake caused tumors to appear as bright images on MRI scans of mice.
“GlucoCEST uses radio waves to magnetically label glucose in the body, said lead researcher Dr Simon Walker-Samuel, from the UCL Center for Advanced Biomedical Imaging (CABI).
“The method uses an injection of normal sugar and could offer a cheap, safe alternative to existing methods for detecting tumors, which [currently] require the injection of radioactive material.” The research could allow vulnerable patient groups such as pregnant women and young children to be scanned more regularly, without the risks associated with a dose of radiation.
Trials are now underway to detect glucose in human cancers.
The work was supported by public and charitable funding from the National Institute for Health Research University College London Hospitals Biomedical Research Center, Cancer Research UK, Engineering and Physical Sciences Research Council (EPSRC) and the British Heart Foundation (BHF).
* According to the Nature Medicine paper, GlucoCEST utilizes two properties of hydroxyl protons: first, when exposed to a magnetic field, the magnetic moments of hydroxyl protons precess at a different frequency as those of bulk tissue water and can therefore be selectively labeled using radiofrequency pulses; second, hydroxyl and water protons undergo exchange, thereby allowing magnetic labeling to be transferred from glucose to water and for glucose to be detected from the change in water signal in the MRI images. The CEST technique thus provides an amplification of detection by using the very large water signal rather than relying on the much smaller signal from glucose.