Large-scale DARPA-funded brain-research program seeks to reduce the severity of neuropsychological illness in service members and veterans
May 28, 2014
DARPA’s SUBNETS program seeks new neurotechnology for analyzing neuronal activity across sub-networks of the brain to enable next-generation therapies tailored to individual patients (credit: DARPA)
Work on DARPA’s Systems-Based Neurotechnology for Emerging Therapies (SUBNETS) program is set to officially launch on June 1, 2014, with teams led by UC San Francisco (UCSF) and Massachusetts General Hospital (MGH).
The $26 million, multi-institutional research program was announced last October in support of President Obama’s Brain initiative.
The SUBNETS program seeks to reduce the severity of neuropsychological illness in service members and veterans by combining recording and analysis of brain activity with near-real-time neural stimulation, using Deep Brain Stimulation (DBS) technology, to coax the brain to “unlearn” the detrimental signaling patterns that underlie these diseases.
UCSF and MGH will oversee teams of physicians, engineers, and neuroscientists who are working together to develop advanced brain interfaces, computational models of neural activity, and clinical therapies for treating networks of the brain.
The teams will collaborate with commercial industry and government, including researchers from Lawrence Livermore National Laboratory and Medtronic, to apply a broad range of perspectives to the technological challenges involved.
SUBNETS is premised on the understanding that brain function — and dysfunction, in the case of neuropsychological illness — plays out across distributed neural systems, as opposed to being strictly relegated to distinct anatomical regions of the brain.
Funded through President Obama’s Brain Initiative, a team of scientists and physicians is embarking on a $26 million project to develop a revolutionary and long-lasting treatment for depression, anxiety disorders, addiction and other neuropsychiatric disorders. The ambitious program led by UCSF also involves UC Berkeley, Lawrence Livermore National Laboratory, Cornell University and New York University, as well as industry partners Posit Science and Cortera Neurotechnologies.
The program also aims to take advantage of neural plasticity, a feature of the brain by which the organ’s anatomy and physiology can alter over time to support normal brain function. Plasticity runs counter to previously held ideas that the adult brain is a “finished” entity that can be statically mapped. Because of plasticity, researchers are optimistic that the brain can be trained or treated to restore normal functionality following injury or the onset of neuropsychological illness.
“The brain is very different from all other organs because of its networking and adaptability,” said Justin Sanchez, the DARPA program manager for SUBNETS. “Real-time, closed-loop neural interfaces allow us to move beyond the traditional static view of the brain and into a realm of precision therapy.
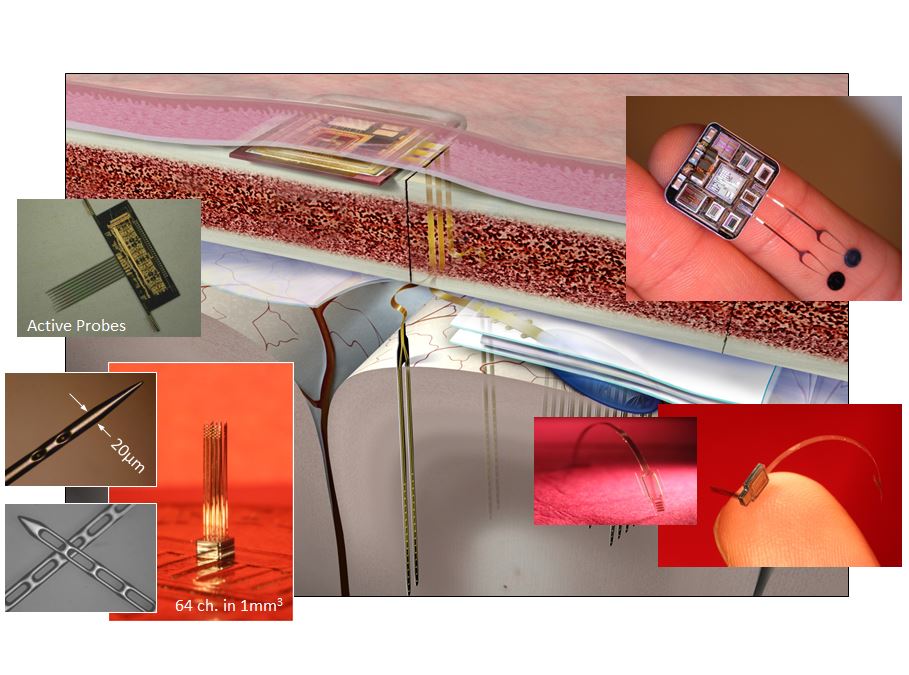
In this artist’s concept, a miniature electronic device placed between a patient’s skull and scalp would serve as an interface between a series of electrodes — placed at varying depths in different regions of the brain — and a clinician, who could wirelessly review neurological data recorded by the electrodes and communicate with the device to prescribe tailored therapies. Photos on either side show a sampling of existing devices that could serve as inspiration or building blocks for SUBNETS technologies. DARPA will evaluate multiple designs from both performer teams over the course of the program. (Credit: Massachusetts General Hospital and Draper Labs)
“This lack of understanding of how mental illness specifically manifests in the brain has limited the effectiveness of existing treatment options, but through SUBNETS we hope to change that. DARPA is looking for ways to characterize which regions come into play for different conditions — measured from brain networks down to the single neuron level — and develop therapeutic devices that can record activity, deliver targeted stimulation, and most importantly, automatically adjust therapy as the brain itself changes.
“The research teams we selected for SUBNETS will pursue bold approaches to reach those goals and we’re excited to get started because this research could prove to be transformative for people with mental illness.”
Team approaches
The UCSF team’s approach is to develop a device that focuses on regions of the brain involved in an individual’s psychiatric or neurologic disease. The device will use direct recording, stimulation, and therapeutic approaches to encourage neural plasticity, with the aim of rehabilitating the circuits that appear to be driving pathology and free an individual from psychiatric or neurologic symptoms. If successful, the approach would allow for the eventual removal of the device.
UCSF’s physician-researchers will begin recording activity in diverse brain regions in people with Parkinson’s disease and medically intractable epilepsy who are already undergoing brain recordings as part of their clinical care, taking advantage of the fact—not well recognized by the public—that neuropsychiatric symptoms are common features of both conditions.
The overall strategy is to first identify brain signaling pathways specifically associated with anxiety and depression, then to develop devices to provide precise stimulation therapies that guide the brain to strengthen alternative circuits. By leveraging the brain’s natural capacity for neural remodeling and learning, this approach will potentially allow the newly strengthened circuits to bypass the disease-associated signals and thereby eliminate symptoms.
The MGH team will pursue a “trans-diagnostic” approach to assessing common components of psychiatric and neurologic diseases — traits common to many such syndromes, including increased anxiety, impaired recall, or inappropriate reactions to stimuli — through qualitative and quantitative behavioral testing combined with high-fidelity, real-time single-neuron recordings.
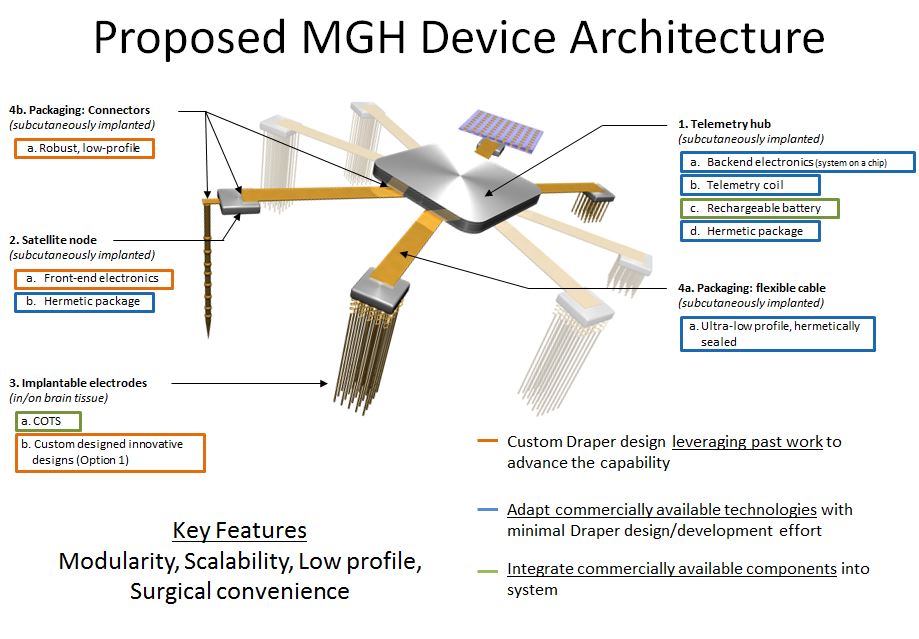
(Artist Concept) The research team led by Massachusetts General Hospital will use a combination of commercial-off-the-shelf electrodes and custom technology developed by Draper Labs to create novel systems. The proposed design will focus on an ultra-low-profile, hermetically sealed interface device capable of being recharged through inductive coupling. (Image courtesy of Massachusetts General Hospital and Draper Labs)
If successful, this method will allow investigators to follow the traces of pathology from individually firing neurons, up through imaging studies of neural network behavior, and into tests that can be performed in the clinical setting. It could also lead to more targeted treatments for psychiatric disease and advance clinicians’ ability to make accurate diagnoses. The MGH team will also work with Draper Laboratories to deploy state-of-the-art advances in micro-fabrication of electronics, with the goal of generating a sophisticated, implantable device that will remain safe and effective through the lifetime of the recipient.
Researchers at UC Berkeley, Cornell University, and New York University will also be involved. Engineers from UC Berkeley and Lawrence Livermore National Laboratory have already made headway in developing a state-of-the-art neuromodulation medical device for this project. Called OMNI, the device consists of low-power, miniaturized electronics that sense and stimulate neural networks to counteract dysfunctional circuits.
Five-year program
The SUBNETS program plan calls for research to be conducted over the next five years along a schedule of prescribed milestones, culminating in technology demonstrations and submission of devices for approval by the U.S. Food and Drug Administration.
“DARPA is in the business of creating not just science, but new technologies,” Sanchez said. “The neurotechnologies we will work to develop under SUBNETS could give new tools to the medical community to treat patients who don’t respond to other therapies, and new knowledge to the neuroscience community to expand the understanding of brain function. We believe this will be a foundational program.”
The Brain Initiative, unveiled in April 2013, is a $100 million program designed to accelerate understanding of human brain function and to fund new technologies to tackle neurological and psychiatric diseases.