Neuroscientists restore vegetative-state patient’s consciousness with vagus nerve stimulation
September 25, 2017
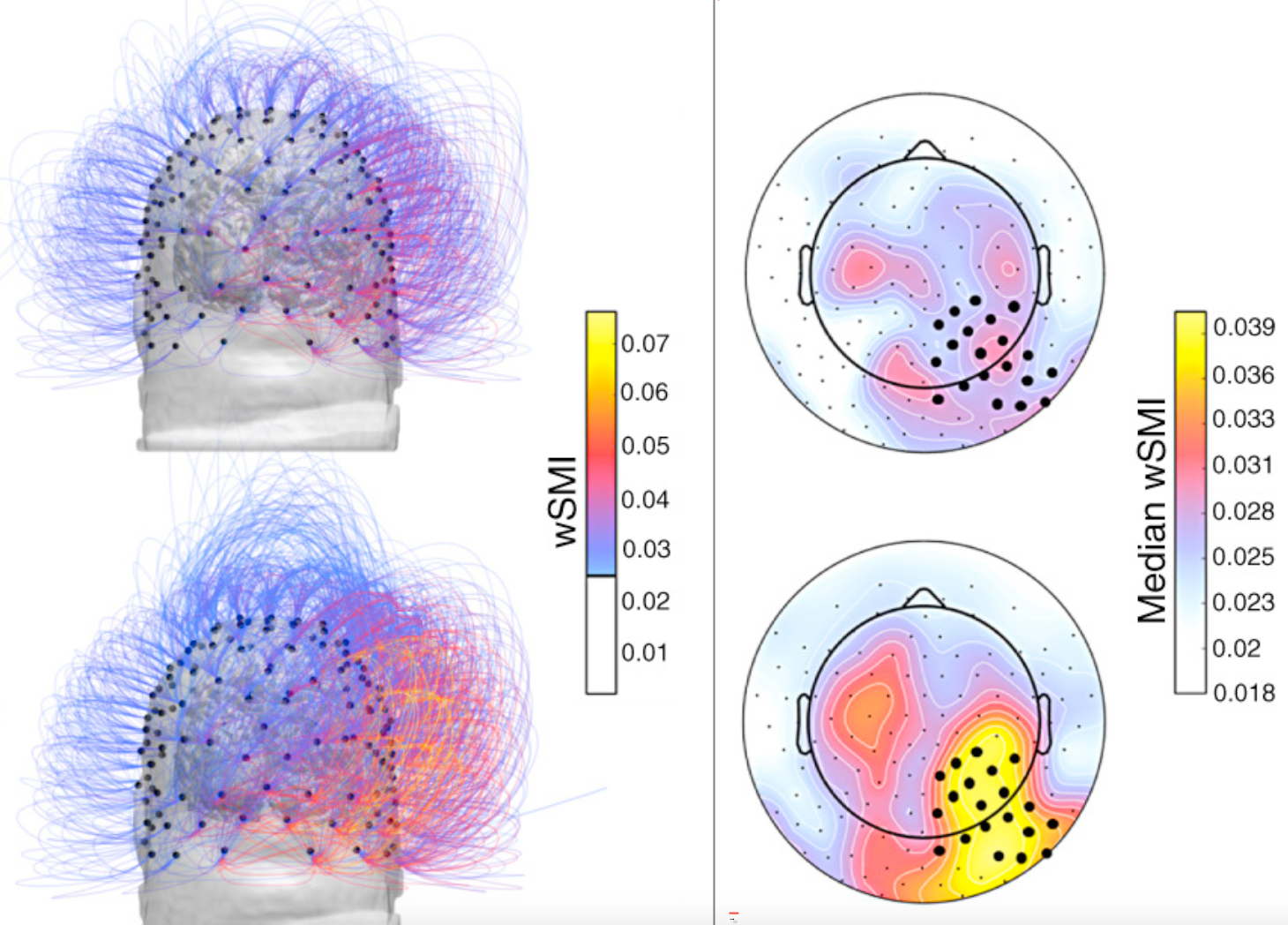
Information sharing increases after vagus nerve stimulation over centroposterior regions of the brain. (Left) Coronal view of weighted symbolic mutual information (wSMI) shared by all channels pre- and post-vagus nerve stimulation (VNS) (top and bottom, respectively). For visual clarity, only links with wSMI higher than 0.025 are shown. (Right) Topographies of the median wSMI that each EEG channel shares with all the other channels pre- and post-VNS (top and bottom, respectively). The bar graph represents the median wSMI over right centroposterior electrodes (darker dots) which significantly increases post-VNS. (credit: Martina Corazzol et al./Current Biology)
A 35-year-old man who had been in a vegetative state for 15 years after a car accident has shown signs of consciousness after neurosurgeons in France implanted a vagus nerve stimulator into his chest — challenging the general belief that disorders of consciousness that persist for longer than 12 months are irreversible.
In a 2007 Weill Cornell Medical College study reported in Nature, neurologists found temporary improvements in patients in a state of minimal consciousness while being treated with bilateral deep brain electrical stimulation (DBS) of the central thalamus. Aiming instead to achieve permanent results, the French researchers proposed use of vagus nerve stimulation* (VNS) to activate the thalamo-cortical network, based on the “hypothesis that vagus nerve stimulation functionally reorganizes the thalamo-cortical network.”
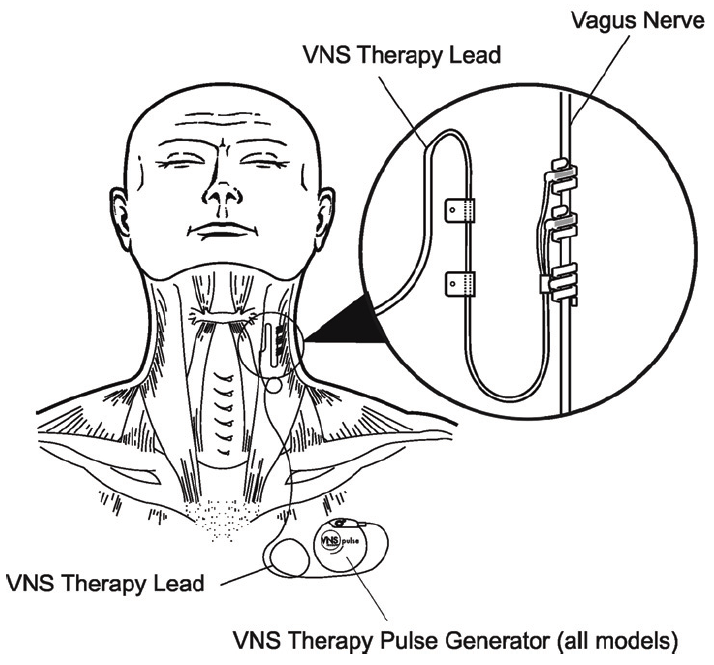
A vagus neural stimulation therapy system. The vagus nerve connects the brain to many other parts of the body, including the gut. It’s known to be important in waking, alertness, and many other essential functions. (credit: Cyberonics, Inc./LivaNova)
After one month of VNS — a treatment currently used for epilepsy and depression — the patient’s attention, movements, and brain activity significantly improved and he began responding to simple orders that were impossible before, the researchers report today (Sept. 25, 2017) in an open-access paper in Current Biology.
For example, he could follow an object with his eyes and turn his head upon request, and when the examiner’s head suddenly approached the patient’s face, he reacted with surprise by opening his eyes wide.
Evidence from brain-activity recordings
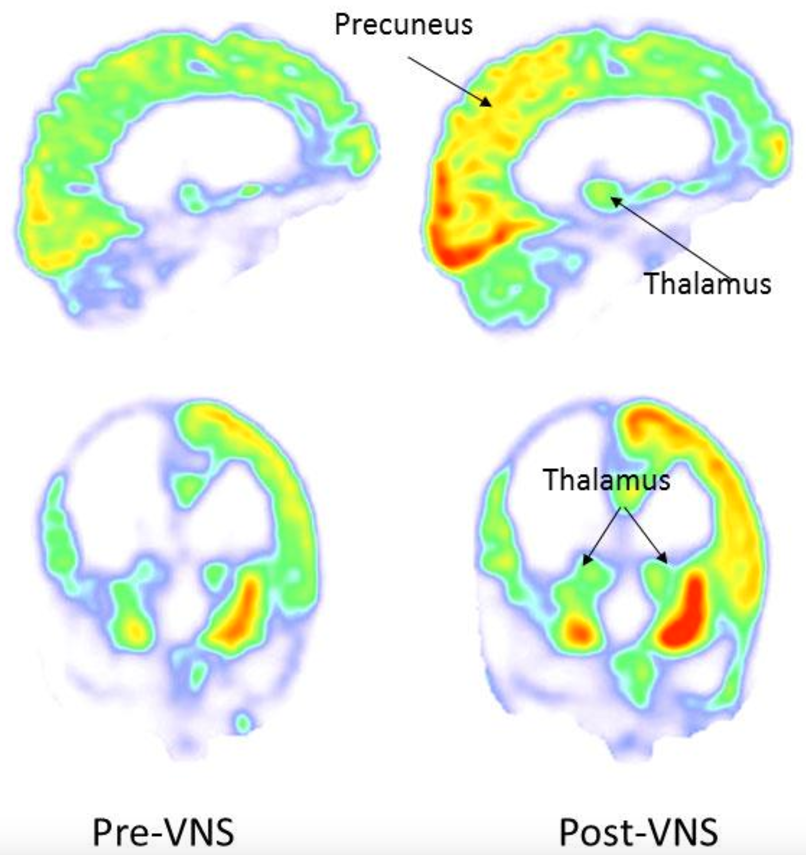
PET images acquired during baseline (left: pre-VNS) and 3 months post vagus nerve stimulation (right: post-VNS). After vagus nerve stimulation, the metabolism increased in the right parieto-occipital cortex, thalamus and striatum. (credit: Corazzol et al.)
“After one month of stimulation, when [electrical current] intensity reached 1 mA, clinical examination revealed reproducible and consistent improvements in general arousal, sustained attention, body motility, and visual pursuit,” the researchers note.
Brain-activity recordings in the new study revealed major changes. A theta EEG signal (important for distinguishing between a vegetative and minimally conscious state) increased significantly in those areas of the brain involved in movement, sensation, and awareness. The brain’s functional connectivity also increased. And a PET scan showed increases in metabolic activity in both cortical and subcortical regions of the brain.
The researchers also speculate that “since the vagus nerve has bidirectional control over the brain and the body, reactivation of sensory/visceral afferences might have enhanced brain activity within a body/brain closed loop process.”
The team is now planning a large collaborative study to confirm and extend the therapeutic potential of VNS for patients in a vegetative or minimally conscious state.
However, “some physicians and brain injury specialists remain skeptical about whether the treatment truly worked as described,” according to an article today in Science. “The surgery to implant the electrical stimulator, the frequent behavioral observations, and the moving in and out of brain scanners all could have contributed to the patient’s improved state, says Andrew Cole, a neurologist at Harvard Medical School in Boston who studies consciousness. ‘I’m not saying their claim is untrue,’ he says. ‘I’m just saying it’s hard to interpret based on the results as presented.’”
The study was supported by CNRS, ANR, and a grant from the University of Lyon
* “The vagus nerve carries somatic and visceral efferents and afferents distributed throughout the central nervous system, either monosynaptically or via the nucleus of the solitary tract (NTS). The vagus directly modulates activity in the brainstem and via the NTS it reaches the dorsal raphe nuclei, the thalamus, the amygdala, and the hippocampus. In humans, vagus nerve stimulation increases metabolism in the forebrain, thalamus and reticular formation. It also enhances neuronal firing in the locus coeruleus which leads to massive release of norepinephrine in the thalamus and hippocampus, a noradrenergic pathway important for arousal, alertness and the fight-or-flight response.” — Corazzol and Lio et al./Current Biology
Abstract of Restoring consciousness with vagus nerve stimulation
Patients lying in a vegetative state present severe impairments of consciousness [1] caused by lesions in the cortex, the brainstem, the thalamus and the white matter [2]. There is agreement that this condition may involve disconnections in long-range cortico–cortical and thalamo-cortical pathways [3]. Hence, in the vegetative state cortical activity is ‘deafferented’ from subcortical modulation and/or principally disrupted between fronto-parietal regions. Some patients in a vegetative state recover while others persistently remain in such a state. The neural signature of spontaneous recovery is linked to increased thalamo-cortical activity and improved fronto-parietal functional connectivity [3]. The likelihood of consciousness recovery depends on the extent of brain damage and patients’ etiology, but after one year of unresponsive behavior, chances become low [1]. There is thus a need to explore novel ways of repairing lost consciousness. Here we report beneficial effects of vagus nerve stimulation on consciousness level of a single patient in a vegetative state, including improved behavioral responsiveness and enhanced brain connectivity patterns.