Paralyzed man walks, thanks to pioneering cell transplanation
October 22, 2014
Darek Fidyka, who was paralyzed from the chest down following a knife attack, can now walk, using a frame, thanks to a pioneering cell transplantation treatment developed by scientists at University College London (UCL) and applied by surgeons at Wroclaw University Hospital, Poland.
The technique, developed by UK research team leader Professor Geoff Raisman, Chair of Neural Regeneration at the UCL Institute of Neurology, involved implanting olfactory ensheathing cells (OECs) from the brain in the spinal cord. These allow the nerve cells that give us a sense of smell to grow back when they are damaged.

An 8mm gap in the right spinal-cord lateral column (credit: Pawel Tabakow et al./Cell Transplantation)
Fidyka was paralyzed after suffering stab wounds to the back in 2010, leaving an 8mm gap in his spinal cord. “It’s amazing to see how regeneration of the spinal cord, something that was thought impossible for many years, is becoming a reality,” said Pawel Tabakow, M.D., a consultant neurosurgeon at Wroclaw University Hospital who led the Polish research team.
Professor Raisman first discovered OECs in 1985 and successfully showed that they could be used to treat spinal injuries in rats in 1997. He has spent the past decade developing OEC spinal repair techniques for patients.
“I believe we have now opened the door to a treatment of spinal cord injury that will get patients out of wheel chairs,” he said. “Our goal now is to develop this first procedure to a point where it can be rolled out as a worldwide general approach.”
The surgery
For the experimental treatment, Fidyka first underwent brain surgery to remove one of his neural olfactory bulbs, the main source of OECs. (These cells help us to distinguish smells, but in this case Darek did not lose his sense of smell.)
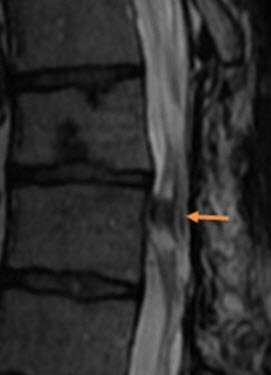
MRI of spinal cord 17 months after operation. Orange arrow: implanted nerve strips. (Credit: Pawel Tabakow et al./Cell Transplantation)
The olfactory bulb was placed in a cell culture for two weeks to produce OECs. These were then injected into the spinal cord above and below the injury, and four strips of nerve tissue were taken from the ankle and patched across the 8mm gap. These formed “bridges” for the spinal nerve fibers to grow across with the aid of OECs.
Three months after the surgery, Darek’s left thigh muscle began to grow and after six months he was starting to walk within the rehabilitation center with the help of a physiotherapist and leg braces. Now, two years on, he is able to walk using a frame, although it is tiring.
His bladder sensation and sexual function have also improved. “I think it’s realistic that one day I will become independent, he said. “What I have learned is that you must never give up but keep fighting, because some door will open in life.”
The research is published in an open-access paper in the journal Cell Transplantation and was jointly funded by the UK Stem Cell Foundation and the Nicholls Spinal Injury Foundation.
The process was documented in a BBC Panorama documentary, “To Walk Again,” broadcast at 22:30 on BBC One on Tuesday October 21, 2014.
Abstract of Functional regeneration of supraspinal connections in a patient with transected spinal cord following transplantation of bulbar olfactory ensheathing cells with peripheral nerve bridging
Treatment of patients sustaining a complete spinal cord injury remains an unsolved clinical problem because of the lack of spontaneous regeneration of injured central axons. A 38-year-old man sustained traumatic transection of the thoracic spinal cord at upper vertebral level Th9. At 21 months after injury the patient presented symptoms of a clinically complete spinal cord injury (American Spinal Injury Association class A-ASIA A). One of the patient’s olfactory bulbs was removed and used to derive a culture containing olfactory ensheathing cells and olfactory nerve fibroblasts. Following resection of the glial scar the cultured cells were transplanted into the spinal cord stumps above and below the injury, and the 8 mm gap bridged by 4 strips of autologous sural nerve. The patient underwent an intense pre- and post-operative neurorehabilitation program. No adverse effects were seen at 19 months postoperatively, and unexpectedly, the removal of the olfactory bulb did not lead to persistent unilateral anosmia. The patient improved from ASIA A to ASIA C. There was improved trunk stability, partial recovery of the voluntary movements of the lower extremities, and an increase of the muscle mass in the left thigh, as well as partial recovery of superficial and deep sensation. There was also some indication of improved visceral sensation and improved vascular autoregulation in the left lower limb. The pattern of recovery suggests functional regeneration of both efferent and afferent long-distance fibers. Imaging confirmed that the grafts had bridged the left side of the spinal cord, where the majority of the nerve grafts were implanted, and neurophysiological examinations confirmed the restitution of the integrity of the corticospinal tracts and the voluntary character of recorded muscle contractions. To our knowledge, this is the first clinical indication of beneficial effects of transplanted autologous bulbar cells.
