Robotic-assisted prostate surgery offers better cancer control, study finds
March 5, 2014
An observational study from UCLA‘s Jonsson Comprehensive Cancer Center has found that prostate cancer patients who undergo robotic-assisted prostate surgery have fewer instances of cancer cells at the edge of their surgical specimen and less need for additional cancer treatments like hormone or radiation therapy than patients who have traditional “open” surgery.
The study, published online Feb. 19 in the journal European Urology, was led by Dr. Jim Hu, UCLA’s Henry E. Singleton Professor of Urology and director of robotic and minimally invasive surgery in the urology department at the David Geffen School of Medicine at UCLA.
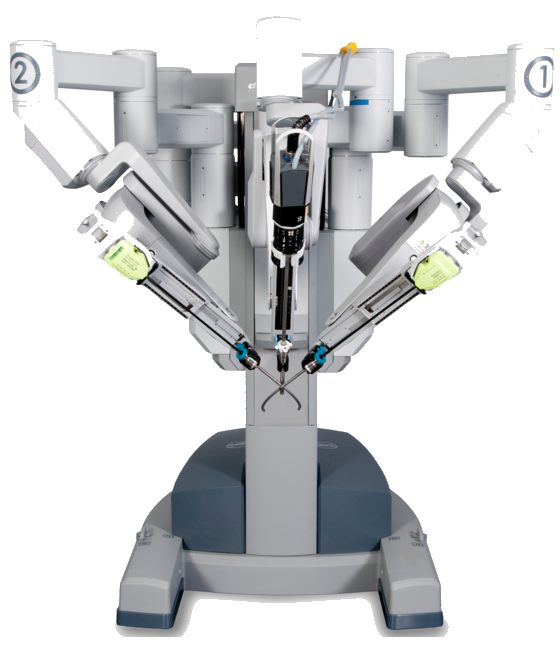
Although it is becoming more popular, robotic-assisted radical prostatectomy — the complete removal of the prostate using a robotic apparatus — remains controversial because there has been little evidence that it provides better cancer control than open radical prostatectomy, the traditional surgical approach, which is less costly.
In an effort to determine whether or not robotic surgery offered an advantage, Hu and his colleagues compared 5,556 patients who received robotic surgery with 7,878 who underwent open surgery between 2004 and 2009. Data was provided by the Surveillance, Epidemiology, and End Results–Medicare, a program of cancer registries that collect clinical and demographic information on people with cancer.
The researchers looked at the surgical margin status of the two groups, which is the amount of cancer cells at the edge of the removed prostate specimen. A positive margin — the presence of cancer cells at the edge — may result from cutting through the cancer and leaving some behind rather than cutting around the cancer completely. In prostate cancer, this has been shown to lead to a greater risk of recurrence and death from the disease.
The team also assessed the use of additional cancer therapies — a hormone therapy known as androgen deprivation, as well as radiation — after robotic surgery and open surgery.
They found that robotic prostate surgery was associated with 5 percent fewer positive margins (13.6 percent vs. 18.3 percent); this difference was greater for patients with intermediate and high-risk prostate cancer. Patients who had robotic surgery also had a one-third reduction in the likelihood of needing additional cancer therapies within 24 months after surgery.
Despite the greater up-front cost of robotic surgery, the findings show that the procedure may translate into less downstream costs and fewer side effects from radiation and hormone therapy, the researchers said.
Abstract of European Urology paper
Background – Robot-assisted radical prostatectomy (RARP) remains controversial, and no improvement in cancer control outcomes has been demonstrated over open radical prostatectomy (ORP).
Objective – To examine population-based, comparative effectiveness of RARP versus ORP surgical margin status and use of additional cancer therapy.
Design, setting, and participants – This was a retrospective observational study of 5556 RARP and 7878 ORP cases from 2004 to 2009 from Surveillance Epidemiology and End Results–Medicare linked data.
Intervention – RARP versus ORP.
Outcome measurements and statistical analysis – Propensity-based analyses were performed to minimize treatment selection biases. Generalized linear regression models were computed for comparison of RP surgical margin status and use of additional cancer therapy (radiation therapy [RT] or androgen deprivation therapy [ADT]) by surgical approach.
Results and limitations – In the propensity-adjusted analysis, RARP was associated with fewer positive surgical margins (13.6% vs 18.3%; odds ratio [OR]: 0.70; 95% confidence interval [CI], 0.66–0.75), largely because of fewer RARP positive margins for intermediate-risk (15.0% vs 21.0%; OR: 0.66; 95% CI, 0.59–0.75) and high-risk (15.1% vs 20.6%; OR: 0.70; 95% CI, 0.63–0.77) disease. In addition, RARP was associated with less use of additional cancer therapy within 6 mo (4.5% vs 6.2%; OR: 0.75; 95% CI, 0.69–0.81), 12 mo (OR: 0.73; 95% CI, 0.62–0.86), and 24 mo (OR: 0.67; 95% CI, 0.57–0.78) of surgery. Limitations include the retrospective nature of the study and the absence of prostate-specific antigen levels to determine biochemical recurrence.
Conclusions – RARP is associated with improved surgical margin status relative to ORP for intermediate- and high-risk disease and less use of postprostatectomy ADT and RT. This has important implications for quality of life, health care delivery, and costs.
Patient summary – Robot-assisted radical prostatectomy (RP) versus open RP is associated with fewer positive margins and better early cancer control because of less use of additional androgen deprivation and radiation therapy within 2 yr of surgery.