‘Shape-memory polymer’ material could help reconstruct faces
August 18, 2014

A new material that changes shape upon heating could help heal bone lesions such as cleft palates, caused by injuries, tumor removal, or birth defects (scale bar: 1 cm.) (credit: Melissa Grunlan, Ph.D.)
Texas A&M University researchers have developed a “self-fitting” material that expands with warm salt water to precisely fill bone defects and also acts as a scaffold for new bone growth, as they reported last week at the 248th National Meeting and Exposition of the American Chemical Society.
Currently, the most common method for filling bone defects in the head, face or jaw (known as the cranio-maxillofacial area) is autografting. That is a process in which surgeons harvest bone from elsewhere in the body, such as the hip bone, and then try to shape it to fit the bone defect.
“The problem is that the autograft is a rigid material that is very difficult to shape into these irregular defects,” says Melissa Grunlan, Ph.D., leader of the study.
Also, harvesting bone for the autograft can itself create complications at the place where the bone was taken.
Another approach is to use bone putty or cement to plug gaps. However, these materials aren’t ideal. They become very brittle when they harden, and they lack pores, or small holes, that would allow new bone cells to move in and rebuild the damaged tissue.
Shape-memory polymer solution
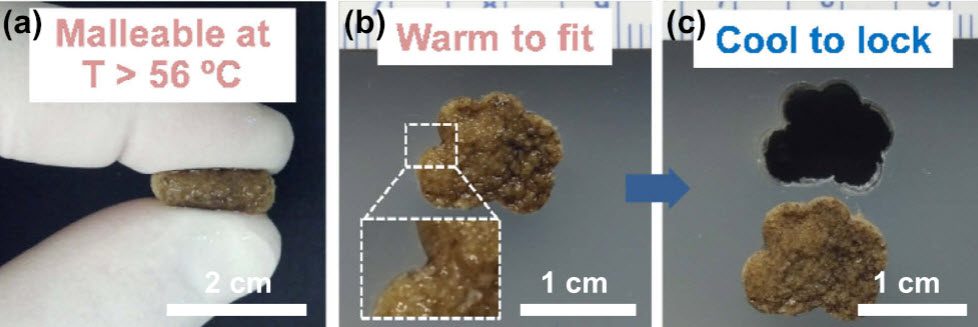
Self-fitting behavior of a polymer scaffold (credit: Dawei Zhang et al./Acta Biomaterialia)
To develop a better material, Grunlan and her colleagues at made a shape-memory polymer (SMP) that molds itself precisely to the shape of the bone defect without being brittle. It also supports the growth of new bone tissue.
SMPs are materials whose geometry changes in response to heat. The team made a porous SMP foam by linking together molecules of poly(ε-caprolactone), an elastic, biodegradable substance that is already used in some medical implants. The resulting material resembled a stiff sponge, with many interconnected pores to allow bone cells to migrate in and grow.
Upon heating to 140 degrees Fahrenheit, the SMP becomes very soft and malleable. So, during surgery to repair a bone defect, a surgeon could warm the SMP to that temperature and fill in the defect with the softened material. Then, as the SMP is cooled to body temperature (98.6 degrees Fahrenheit), it would resume its former stiff texture and “lock” into place.
The researchers also coated the SMPs with polydopamine, a sticky substance that helps lock the polymer into place by inducing formation of a mineral that is found in bone. It may also help osteoblasts, the cells that produce bone, to adhere and spread throughout the polymer. The SMP is biodegradable, so that eventually the scaffold will disappear, leaving only new bone tissue behind.
To test whether the SMP scaffold could support bone cell growth, the researchers seeded the polymer with human osteoblasts (cells with single nuclei that synthesize bone). After three days, the polydopamine-coated SMPs had grown about five times more osteoblasts than those without a coating. Furthermore, the osteoblasts produced more of the two proteins, runX2 and osteopontin, that are critical for new bone formation.
Grunlan says that the next step will be to test the SMP’s ability to heal cranio-maxillofacial bone defects in animals. “The work we’ve done in vitro is very encouraging,” she says. “Now we’d like to move this into preclinical and, hopefully, clinical studies.”
“To heal bone defects, the material — whether it is a biological autograft or a synthetic material — must achieve a very good fit with the adjacent bone tissue,” Grunlan explained to KurzweilAI in an email interview.
“If good contact isn’t achieved, healing is compromised. Because of the ‘shape memory’ or ‘shape shifting’ ability of this foam, it can be easily fit into an irregular bone defect by merely first soaking the foam in warm saline. Once “set” in the bone defect, it will cool and become rigid again, locking in the new shape. This self-fitting property distinguishes our material from most other approaches.”
The researchers acknowledge funding from the Texas A&M Engineering Experiment Station.
Abstract of Acta Biomaterialia paper
While tissue engineering is a promising alternative for treating critical-sized cranio-maxillofacial bone defects, improvements in scaffold design are needed. In particular, scaffolds that can precisely match the irregular boundaries of bone defects as well as exhibit an interconnected pore morphology and bioactivity would enhance tissue regeneration. In this study, a shape memory polymer (SMP) scaffold was developed exhibiting an open porous structure and the capacity to conformally “self-fit” into irregular defects. The SMP scaffold was prepared via photocrosslinking of poly(ε-caprolactone) (PCL) diacrylate using a SCPL method, which included a fused salt template. A bioactive polydopamine coating was applied to coat the pore walls. Following exposure to warm saline at T > Ttrans (Ttrans = Tm of PCL), the scaffold became malleable and could be pressed into an irregular model defect. Cooling caused the scaffold to lock in its temporary shape within the defect. The polydopamine coating did not alter the physical properties of the scaffold. However, polydopamine-coated scaffolds exhibited superior bioactivity (i.e. formation of hydroxyapatite in vitro), osteoblast adhesion, proliferation, osteogenic gene expression and extracellular matrix deposition.