Why cancer rate increases with age (not mutations)
July 3, 2012

(Credit: stock image)
It is the changing features of tissue in old age that promote higher cancer rates in the elderly, not the accumulation of cancer-causing mutations, concludes a University of Colorado Cancer Center review.
“If you look at Mick Jagger in 1960 compared to Mick Jagger today, it’s obvious that his tissue landscape has changed,” says James DeGregori, PhD, investigator at the University of Colorado Cancer Center and professor of molecular biology at the University of Colorado School of Medicine. “And it’s this change, not the accumulation of cancer-causing mutations, that drives cancer rates higher as we grow older.”
For evidence, DeGregori points first to the fact that by the time we stop growing in our late teens, we’ve already accumulated a large fraction of the mutations we will have in our lifetimes.
“There’s a mismatch between the mutation curve and the cancer curve,” DeGregori says, meaning that if cancer were due to reaching a tipping point of, say, five or six mutations, we should see higher cancer rates in 20-year-olds, as this is when mutation rate is highest.
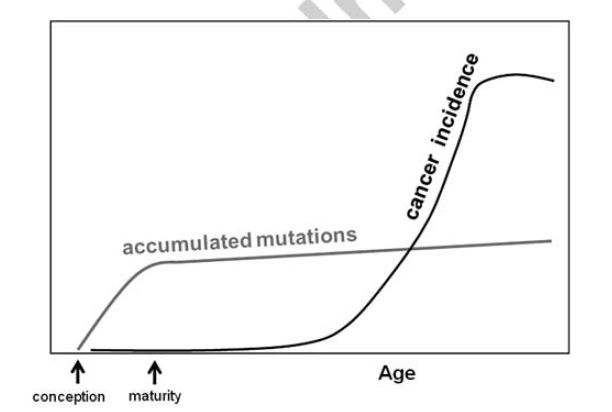
Comparison of the time courses of mutation accumulation with onset of malignancies in the hematopoietic system in mice (credit: J DeGregori/Oncogene)
Second, DeGregori points out that even healthy tissues are full of oncogenic mutations. “These mutations are many times more common than the cancers associated with them,” DeGregori says. Simply, more mutations doesn’t equal more cancer — not across the aging population and not even in specific tissues.
DeGregori’s final two points come from evolution. As we’ve evolved from one-celled, short-lived life forms into multicellular, long-lived humans, we’ve had to develop complicated machinery to maintain our tissues and avoid disease.
“But we’re no better at preventing mutations than our yeast or bacteria cousins,” DeGregori says. “You’d think if avoiding mutations was key to avoiding cancer, we’d be better at it than we are.”
And finally, if these oncogenes were the evil super-villains they’ve been made out to be, capable of taking over surrounding tissue, then introducing oncogenes into mice stem cells should help rather than hurt these cells’ survival. “Rather, stem cells harboring the oncogenes tend to get weeded out,” says DeGregori.
Instead of gathering mutations until they give us cancer, DeGregori says that as we age, the mechanisms that younger adults use to fight cancer deteriorate.
“It’s like what happened to the dinosaurs 65 million years ago,” DeGregori says. “Dinosaurs were great and they weren’t changing that fast. They were well adapted to their landscape. Until that darn meteor. Suddenly what was fit was no longer fit. The species didn’t have to change their mutation rate — it was the new landscape that drove speciation. Similarly, what primarily drives cancer rates higher as we age is the changed landscape.”
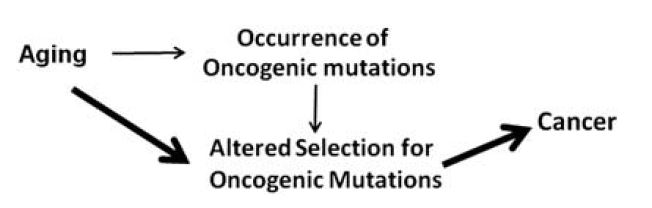
Selection-centric model. This model posits that aging is largely associated with cancer due to alterations in selection for oncogenic mutations. The weight of the arrow reflects the proposed contribution to cancer incidence. (Credit: J DeGregori/Oncogene)
Our healthy cells are optimized for the conditions of our healthy, younger tissue. Change this balance, as does an oncogenic mutation, and they’re no longer a perfect fit for the surroundings — healthy cells in young bodies quickly outcompete cells with cancerous mutations.
But, “when tissue is old, healthy cells are no longer a perfect fit, and mutations might help a cancer cell adapt in ways a healthy cell can’t,” DeGregori says.
Blot out the sun with a meteor’s cloud of dust and mammals will eventually outcompete thunder lizards. Age tissue past the expiration date evolution’s set and cancer cells can outcompete their normal but aged peers.
Funding was provided in part by grants from the National Institutes of Health (R01- CA157850) and the Leukemia Lymphoma Society.