Scientists track amazing restoration of communication in ‘minimally conscious’ patient
December 10, 2016

Nancy Smith Worthen doing art therapy with her daughter, Maggie, who was initially minimally conscious. (credit: Nancy Worthen)
In a three-year study of a severely brain-injured woman’s remarkable recovery, doctors measured aspects of brain structure and function before and after recovering communication, a first — raising the question: could other minimally responsive or unresponsive chronic-care patients also regain organized, higher-level brain function?
Challenging what neurologists thought was possible, the pioneering study by Weill Cornell Medicine scientists was published Dec. 7 in Science Translational Medicine.
It began 21 months after Margaret Worthen suffered massive strokes. Most doctors diagnosed her as being in a vegetative state, unable to speak and unaware of herself and her environment.
Then, during her first visit with a new team led by senior study author Nicholas D. Schiff, M.D.,* doctors detected an unexpected ability to respond to their command to look down with her left eye.
Her ability was initially intermittent, but over the course of a year she developed a viable one-way communication system. She was able to respond to yes and no questions, such as “Is your name Margaret?” or “Is your father’s name Michael?” by moving her left eye down or up, but still lacked a method to ask questions or use a brain-computer interface.
But over the next nearly two years, the connections and function of the areas of her brain responsible for producing expressive language and responding to human speech were also gradually restored.
To measure the changes in Margaret’s brain as she recovered the ability to communicate, the researchers used a number of state-of-the-art imaging tools. The main technique, called diffusion tensor imaging, uses the diffusion of water molecules to generate contrast in magnetic resonance (MRI) images, enabling scientists to infer the degree of white-matter connection between specific areas.
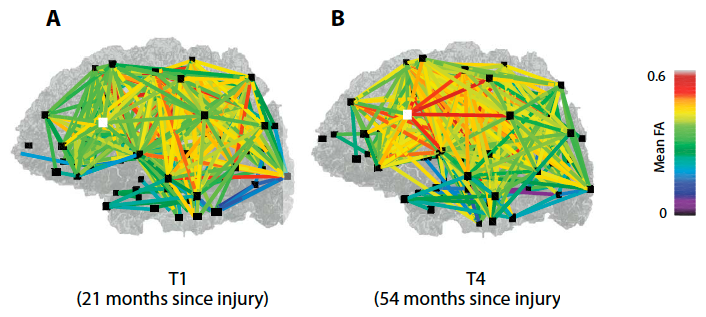
Longitudinal structural remodeling of the brain, as identified by diffusion tensor imaging. The “fractional anisotropy” (FA) between cortical regions, which indicates the concentration in specific white matter fibers — measured (from 0 to 1) at the first (A) and last (B) time point of evaluation — is shown as colored lines between the connected brain regions (black squares), exhibiting a notable increase of connections. The FA changes reflect fiber density, axonal diameter, and myelination (covering) in white matter. The inferior temporal gyrus, which is associated with visual object recognition, is denoted with a white square. (credit: Daniel J. Thengone et al./Science Translation Medicine)
The researchers also found a reconnection of Broca’s area — the region of the brain located in the frontal lobe of the dominant hemisphere that is associated with language and speech. In addition, the two hemispheres of the patient’s brain increased their connectivity. The findings suggest that reconnection began within the left hemisphere and extended to the right, corresponding to the restoration of Worthen’s ability to communicate.
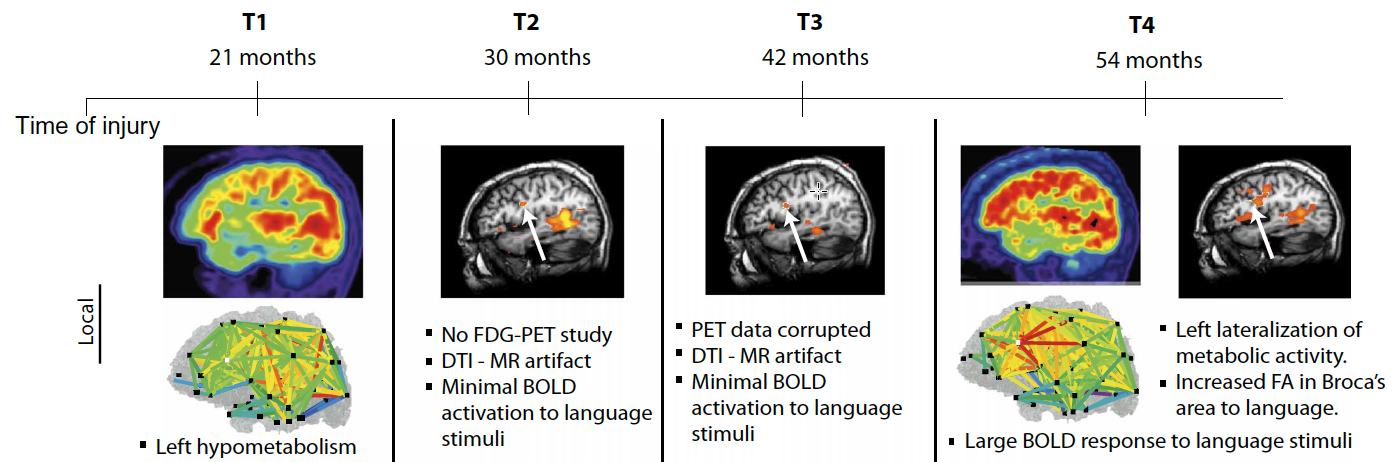
Local and global changes in brain structure and function captured over time using multimodal imaging analyses. The time line shows the four time points of evaluation (T1 to T4) since the patient suffered a traumatic brain injury. From the first time point of evaluation (at 21 months after injury) to the last (at 54 months after injury), structural and functional brain imaging and electrophysiological studies revealed concordant findings in global remodeling and local changes, supporting the recovery of language abilities over the 2-year and 9-month period. Note the increase (more red) in white matter fiber density between 21 and 54 months. (credit: Daniel J. Thengone et al./Science Translation Medicine)
The researchers also used functional MRI (fMRI) to measure blood flow changes in response to brain activity while Ms. Worthen listened to a human voice speaking. They found that the functional recovery of Broca’s area over time corresponded with the change in structural connectivity. In addition, language-responsive brain regions showed increasing correlation across both hemispheres over time.
“She was being treated as if she was there, and she was present.”
What triggered the restoration of her brain’s expressive language system was her caregivers’ attempts to establish communication over the nearly three years of the study. Her recovered expressive language networks may also have triggered a restoration of her inner speech or inner dialogue, which could have reinforced those same networks, according to the study authors.
The findings raise important questions about how clinicians care for patients who are diagnosed as in vegetative or minimally conscious state, Schiff said. “We looked carefully at Margaret, made an observation that there was a way to try to connect with her, and the world changed for her. Her life changed because now she wasn’t being treated as if she may or may not be conscious. She was being treated as if she was there, and she was present.”
The discovery changed everything, according to her mother, Nancy Smith Worthen. For example, it opened the door to speech therapy, which enabled caregivers to assess whether or not she was experiencing pain, and for her mother to determine her daughter’s wants or needs. Margaret was able to produce paintings with her mother’s hand guiding her, which her mother credits with further stimulating her brain.
Margaret went on to develop enough facility with a computer interface that she was actually able to attend her five-year college reunion and hold conversations with classmates, assisted by a speech therapist. Her story is among those included in Rights Come to Mind: Brain Injury, Ethics, and the Struggle for Consciousness, by Joseph Fins, M.D., the E. William Davis Jr., MD, Professor of Medical Ethics and chief of the Division of Medical Ethics at Weill Cornell Medicine.
Regrettably, she died of complications from pneumonia in 2015.
“When I would ask Margaret if she wanted to do this work with Dr. Schiff, she would always say yes,” Nancy Smith Worthen said. “To have her brain be studied was the way she could do something in the world with her disability. And now, even after she’s gone, she’s still contributing. I’m just so proud of her.”
New hope for minimally conscious patients
Although the findings are from a single-subject study, scientists say they could apply to other patients, based on the proposed mechanism and previous research findings. Ten years ago, team members reported similar changes of increased connections between the two cerebral hemispheres in Terry Wallis, a minimally conscious patient who spontaneously recovered speech 19 years after a traumatic brain injury.
In addition, other studies have implicated injuries to the central thalamus such as those Margaret experienced in a general mechanism underlying impaired function in patients with disorders of consciousness.
This research was supported by the National Institutes of Health, the Charles A. Dana Foundation, the James S. McDonnell Foundation, the Jerold B. Katz Foundation and the Fred Plum Fellowship in Systems Neurology and Neurosciences.
* Schiff is the Jerold B. Katz Professor of Neurology and Neuroscience in the Feil Family Brain and Mind Research Institute at Weill Cornell Medicine.
Abstract of Local changes in network structure contribute to late communication recovery after severe brain injury
Spontaneous recovery of brain function after severe brain injury may evolve over a long time period and is likely to involve both structural and functional reorganization of brain networks. We longitudinally tracked the recovery of communication in a patient with severe brain injury using multimodal brain imaging techniques and quantitative behavioral assessments measured at the bedside over a period of 2 years and 9 months (21 months after initial injury). Structural diffusion tensor imaging revealed changes in brain structure across interhemispheric connections and in local brain regions that support language and visuomotor function. These findings correlated with functional brain imaging using functional magnetic resonance imaging and positron emission tomography, which demonstrated increased language network recruitment in response to natural speech stimuli, graded increases in interhemispheric interactions of language-related frontal cortices, and increased cerebral metabolic activity in the language-dominant hemisphere. In addition, electrophysiological studies showed recovery of synchronization of sleep spindling activity. The observed changes suggest a specific mechanism for late recovery of communication after severe brain injury and provide support for the potential of activity-dependent structural and functional remodeling over long time periods.